Monday Poster Session
Category: GI Bleeding
P2105 - Ascending Colonic Varices Resulting in Massive Gastrointestinal Bleed
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kelvin Liao, MD
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Kelvin Liao, MD1, Pei Xue, MD2, Patrick McCarthy, MD1, Stephen Schwartz, DO3, Nathalie Urrunaga, MD2
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland Medical System, Baltimore, MD
Introduction: Gastrointestinal bleeding (GIB) secondary to ruptured varices is a potentially fatal complication of cirrhosis. The most common site of varices is the esophagus followed by the gastric body, although ectopic variceal bleeding can occur in about 2-5% of cases of variceal hemorrhage. We describe a case of a patient who presented with massive lower GIB and was found to have ruptured variceal bleeding located in the ascending colon, which is a rare site of ectopic variceal bleeding.
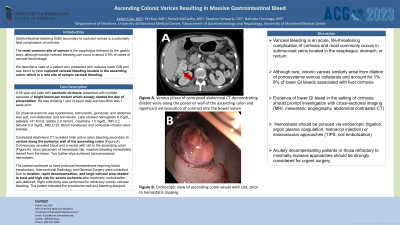
Case Description/Methods: Our patient is a 35-year-old male with alcoholic cirrhosis who presented with massive lower GIB. He had multiple episodes of bright blood per rectum which acutely started the day of presentation. He was drinking 1 pint of liquor daily and last drink was 1 week prior. On physical exam he was hypotensive, tachycardic, jaundiced, and abdomen was soft, non-distended, and non-tender. Labs showed hemoglobin 6.0 g/dL, platelets 141 K/mcl; lactate 2.0 mmol/L, creatinine 1.5 mg/dL; INR 2.2, bilirubin 5.9 mg/dL, MELD 25. Blood transfusion and octreotide infusion were initiated. Contrasted abdominal CT revealed brisk active colon bleeding secondary to varices along the posterior wall of the ascending colon. Colonoscopy revealed blood and a vessel with clot in the ascending colon (Figure 1). Upon placement of hemostatic clip, massive bleeding immediately started from the lesion. Two further clips achieved intra-procedural hemostasis. However, the patient continued to have profound hematochezia requiring blood transfusions. Interventional Radiology and General Surgery were consulted. Due to location, rapid decompensation, and large variceal area needed to treat and high risk for severe ischemia after treatment, embolization was deferred. Right colectomy was performed for refractory colonic variceal bleeding. The patient tolerated the procedures well and bleeding stopped.
Discussion: Variceal bleeding is an acute, life-threatening complication of cirrhosis and most commonly occurs in submucosal veins located in the esophagus, stomach, or rectum. Although rare, colonic varices similarly arise from dilation of portosystemic venous collaterals. Suspected colonic variceal GIB requires prompt initiation of medical management while obtaining contrasted CT and endoscopic evaluation. Hemostasis should be pursued via endoscopic or endovascular approaches. Acutely decompensating patients or those refractory to minimally-invasive approaches should be strongly considered for urgent surgery.

Disclosures:
Kelvin Liao, MD1, Pei Xue, MD2, Patrick McCarthy, MD1, Stephen Schwartz, DO3, Nathalie Urrunaga, MD2. P2105 - Ascending Colonic Varices Resulting in Massive Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland Medical System, Baltimore, MD
Introduction: Gastrointestinal bleeding (GIB) secondary to ruptured varices is a potentially fatal complication of cirrhosis. The most common site of varices is the esophagus followed by the gastric body, although ectopic variceal bleeding can occur in about 2-5% of cases of variceal hemorrhage. We describe a case of a patient who presented with massive lower GIB and was found to have ruptured variceal bleeding located in the ascending colon, which is a rare site of ectopic variceal bleeding.
Case Description/Methods: Our patient is a 35-year-old male with alcoholic cirrhosis who presented with massive lower GIB. He had multiple episodes of bright blood per rectum which acutely started the day of presentation. He was drinking 1 pint of liquor daily and last drink was 1 week prior. On physical exam he was hypotensive, tachycardic, jaundiced, and abdomen was soft, non-distended, and non-tender. Labs showed hemoglobin 6.0 g/dL, platelets 141 K/mcl; lactate 2.0 mmol/L, creatinine 1.5 mg/dL; INR 2.2, bilirubin 5.9 mg/dL, MELD 25. Blood transfusion and octreotide infusion were initiated. Contrasted abdominal CT revealed brisk active colon bleeding secondary to varices along the posterior wall of the ascending colon. Colonoscopy revealed blood and a vessel with clot in the ascending colon (Figure 1). Upon placement of hemostatic clip, massive bleeding immediately started from the lesion. Two further clips achieved intra-procedural hemostasis. However, the patient continued to have profound hematochezia requiring blood transfusions. Interventional Radiology and General Surgery were consulted. Due to location, rapid decompensation, and large variceal area needed to treat and high risk for severe ischemia after treatment, embolization was deferred. Right colectomy was performed for refractory colonic variceal bleeding. The patient tolerated the procedures well and bleeding stopped.
Discussion: Variceal bleeding is an acute, life-threatening complication of cirrhosis and most commonly occurs in submucosal veins located in the esophagus, stomach, or rectum. Although rare, colonic varices similarly arise from dilation of portosystemic venous collaterals. Suspected colonic variceal GIB requires prompt initiation of medical management while obtaining contrasted CT and endoscopic evaluation. Hemostasis should be pursued via endoscopic or endovascular approaches. Acutely decompensating patients or those refractory to minimally-invasive approaches should be strongly considered for urgent surgery.

Figure: Figure 1. (A) Venous phase of abdominal CT with intravenous contrast demonstrating dilated veins along he posterior wall of the ascending colon and significant extravasation of contrast into the bowel lumen, concerning for variceal bleeding. (B) Endoscopic view of ascending colon vessel with clot, prior to hemostatic clipping.
Disclosures:
Kelvin Liao indicated no relevant financial relationships.
Pei Xue indicated no relevant financial relationships.
Patrick McCarthy indicated no relevant financial relationships.
Stephen Schwartz indicated no relevant financial relationships.
Nathalie Urrunaga indicated no relevant financial relationships.
Kelvin Liao, MD1, Pei Xue, MD2, Patrick McCarthy, MD1, Stephen Schwartz, DO3, Nathalie Urrunaga, MD2. P2105 - Ascending Colonic Varices Resulting in Massive Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
