Monday Poster Session
Category: IBD
P2112 - Are Appendectomies Beneficial in Patients With Inflammatory Bowel Disease? A U.S. Nationwide Cohort Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sanket Basida, MD
University of Missouri at Columbia
Columbia, MO
Presenting Author(s)
Sanket Basida, MD1, Mythili Menon Pathiyil, MD2, Muhammad Nadeem. Yousaf, MD3, Yezaz Ghouri, MD4
1University of Missouri at Columbia, Columbia, MO; 2Saint Vincent Hospital, Worcester, MA; 3University of Missouri-Columbia, Columbia, MO; 4University of Missouri School of Medicine, Columbia, MO
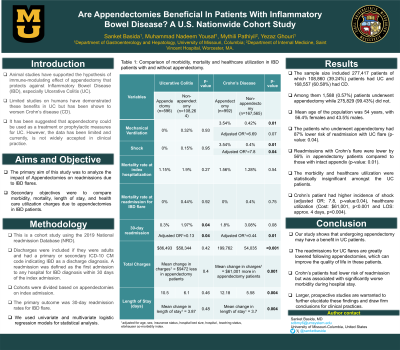
Introduction: Animal studies have supported the hypothesis of immune-modulating effect of appendectomy that protects against Ulcerative Colitis (UC). Limited studies on humans have demonstrated these benefits in UC but has been shown to worsen Crohn’s disease (CD). It has been suggested that appendectomy could be used as a treatment or prophylactic measures for UC. However, the data has been limited. Thus, we sought to analyze the impact of appendectomies on IBD patients.
Methods: This is a cohort study using the 2019 National readmission Database. Discharges were included if they were adults and had a primary or secondary ICD-10 CM code indicating IBD. A readmission was defined as hospitalization due to IBD within 30 days from index admission. Same day admissions and discharges were excluded. The primary outcome was 30-days readmission rates for IBD flare. Secondary outcomes were morbidity, mortality and resource utilization (length of stay and hospitalization total cost). We used univariate and multivariate regression models for statistical analysis.
Results: A total 277,417 patients with 56.4% being female and mean age of 54 years were analyzed. Patients with UC and CD were 108,860 (39.24%) and 168,557 (60.58%) respectively with an overall incidence of elective or non-elective appendectomy 0.57% (n=1,588). On subgroup analysis, 0.55% of UC and 0.59% of CD patients underwent appendectomy. The UC patients with appendectomy had 87% (adjusted OR: 0.13, p-value= 0.04) and CD patients had 56% (adjusted OR:0.44, p-value= 0.01) lower risk of readmission due to flare compared to those with intact appendix. Overall, females had 18% lower risk of developing IBD flares post appendectomy. With increasing age, the risk of developing flare reduced by 3%. The morbidity and healthcare utilization were insignificant in UC patients. CD patient had higher incidence of shock (adjusted odds ratio: 7.8, p-value: 0.04) and healthcare utilization (Cost: $61,001, p< 0.001 and LOS: about 4 days, p< 0.004).
Discussion: Patients with UC has lower risks of readmission rate due to UC flare after appendectomy. CD patients with appendectomy had higher rate of complications during hospital stay and increased healthcare utilization. Larger, prospective studies are warranted to further elucidate these findings and draw firm conclusions for clinical practices.
Disclosures:
Sanket Basida, MD1, Mythili Menon Pathiyil, MD2, Muhammad Nadeem. Yousaf, MD3, Yezaz Ghouri, MD4. P2112 - Are Appendectomies Beneficial in Patients With Inflammatory Bowel Disease? A U.S. Nationwide Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri at Columbia, Columbia, MO; 2Saint Vincent Hospital, Worcester, MA; 3University of Missouri-Columbia, Columbia, MO; 4University of Missouri School of Medicine, Columbia, MO
Introduction: Animal studies have supported the hypothesis of immune-modulating effect of appendectomy that protects against Ulcerative Colitis (UC). Limited studies on humans have demonstrated these benefits in UC but has been shown to worsen Crohn’s disease (CD). It has been suggested that appendectomy could be used as a treatment or prophylactic measures for UC. However, the data has been limited. Thus, we sought to analyze the impact of appendectomies on IBD patients.
Methods: This is a cohort study using the 2019 National readmission Database. Discharges were included if they were adults and had a primary or secondary ICD-10 CM code indicating IBD. A readmission was defined as hospitalization due to IBD within 30 days from index admission. Same day admissions and discharges were excluded. The primary outcome was 30-days readmission rates for IBD flare. Secondary outcomes were morbidity, mortality and resource utilization (length of stay and hospitalization total cost). We used univariate and multivariate regression models for statistical analysis.
Results: A total 277,417 patients with 56.4% being female and mean age of 54 years were analyzed. Patients with UC and CD were 108,860 (39.24%) and 168,557 (60.58%) respectively with an overall incidence of elective or non-elective appendectomy 0.57% (n=1,588). On subgroup analysis, 0.55% of UC and 0.59% of CD patients underwent appendectomy. The UC patients with appendectomy had 87% (adjusted OR: 0.13, p-value= 0.04) and CD patients had 56% (adjusted OR:0.44, p-value= 0.01) lower risk of readmission due to flare compared to those with intact appendix. Overall, females had 18% lower risk of developing IBD flares post appendectomy. With increasing age, the risk of developing flare reduced by 3%. The morbidity and healthcare utilization were insignificant in UC patients. CD patient had higher incidence of shock (adjusted odds ratio: 7.8, p-value: 0.04) and healthcare utilization (Cost: $61,001, p< 0.001 and LOS: about 4 days, p< 0.004).
Discussion: Patients with UC has lower risks of readmission rate due to UC flare after appendectomy. CD patients with appendectomy had higher rate of complications during hospital stay and increased healthcare utilization. Larger, prospective studies are warranted to further elucidate these findings and draw firm conclusions for clinical practices.
Disclosures:
Sanket Basida indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Yezaz Ghouri indicated no relevant financial relationships.
Sanket Basida, MD1, Mythili Menon Pathiyil, MD2, Muhammad Nadeem. Yousaf, MD3, Yezaz Ghouri, MD4. P2112 - Are Appendectomies Beneficial in Patients With Inflammatory Bowel Disease? A U.S. Nationwide Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
