Monday Poster Session
Category: Esophagus
P1898 - A Case of Wernicke’s Encephalopathy Due to Type 2 Achalasia
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DR
Diana N. Rodriguez, MD
UF Health Shands Hospital
Gainesville, FL
Presenting Author(s)
Diana N. Rodriguez, MD1, Kriti Gera, MD1, Vanessa I. Rodriguez, MD2, Angela Pham, MD3
1UF Health Shands Hospital, Gainesville, FL; 2University of South Florida, Tampa, FL; 3University of Florida, Gainesville, FL
Introduction: Achalasia is primarily a motility disorder of the esophagus driven by aberrant peristalsis and failure of sphincter relaxation. Per review of current literature regarding achalasia, patients primarily present with dysphagia, usually to solids and, if progressed, to solids and liquids. Seldomly, untreated achalasia results in thiamine deficiency and presents as Wernicke’s-Korsakoff (WK). This acute neurologic condition affects the central and peripheral nervous system and is known by the triad of ataxia, ophthalmoplegia and confusion. Individuals who present with WK typically have a notable history of chronic alcohol abuse with decreased thiamine intake and metabolism. We highlight a unique presentation of Wernicke’s encephalopathy in a 30-year-old female with severe type II achalasia
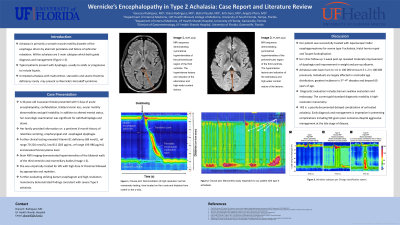
Case Description/Methods: This is a 30-year-old female who presented with acute encephalopathy with confabulation, bilateral loss of vision, ocular motility abnormalities, lower extremity weakness and gait instability over the span of 5 days. She also reported a 5-month history of intractable nausea, vomiting associated with progressive oropharyngeal and esophageal dysphagia associated with 27 kg weight loss. Subsequent brain MRI revealed hyperintensities of the third ventricle walls and mamillary bodies. Her nutrition panel was notable for vitamin B1 deficiency, low B12 and elevated homocysteine level. Appropriate physical exam was limited by lack of cooperation and empiric management for suspected WE and suspected beriberi peripheral neuropathy was initiated. High resolution manometry demonstrated abnormal relaxation of the esophagogastric junction, abnormal relaxation median supine integrative relaxation pressure, hypertensive LES, no normal peristalsis with panesophageal pressurization in all swallows, scattered jackhammer activity and retrograde peristalsis and negligible upper esophageal sphincter tone. She underwent laparoscopic Heller esophagomyotomy for severe type 2 achalasia.
Discussion: Achalasia incidence rates were perceived lower until annual rates have risen to 1.6 per 100000 versus 0.5 - 1.2 per 100000. Achalasia appears to affect individuals by bimodal age distribution at diagnosis with the greatest incidence in the 3rd-4th decade and the other at 60 years of age, close to the median age of our patients with achalasia and WE. This case highlights WE as an atypical presentation of achalasia and outcomes despite aggressive management of late-stage disease.

Disclosures:
Diana N. Rodriguez, MD1, Kriti Gera, MD1, Vanessa I. Rodriguez, MD2, Angela Pham, MD3. P1898 - A Case of Wernicke’s Encephalopathy Due to Type 2 Achalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UF Health Shands Hospital, Gainesville, FL; 2University of South Florida, Tampa, FL; 3University of Florida, Gainesville, FL
Introduction: Achalasia is primarily a motility disorder of the esophagus driven by aberrant peristalsis and failure of sphincter relaxation. Per review of current literature regarding achalasia, patients primarily present with dysphagia, usually to solids and, if progressed, to solids and liquids. Seldomly, untreated achalasia results in thiamine deficiency and presents as Wernicke’s-Korsakoff (WK). This acute neurologic condition affects the central and peripheral nervous system and is known by the triad of ataxia, ophthalmoplegia and confusion. Individuals who present with WK typically have a notable history of chronic alcohol abuse with decreased thiamine intake and metabolism. We highlight a unique presentation of Wernicke’s encephalopathy in a 30-year-old female with severe type II achalasia
Case Description/Methods: This is a 30-year-old female who presented with acute encephalopathy with confabulation, bilateral loss of vision, ocular motility abnormalities, lower extremity weakness and gait instability over the span of 5 days. She also reported a 5-month history of intractable nausea, vomiting associated with progressive oropharyngeal and esophageal dysphagia associated with 27 kg weight loss. Subsequent brain MRI revealed hyperintensities of the third ventricle walls and mamillary bodies. Her nutrition panel was notable for vitamin B1 deficiency, low B12 and elevated homocysteine level. Appropriate physical exam was limited by lack of cooperation and empiric management for suspected WE and suspected beriberi peripheral neuropathy was initiated. High resolution manometry demonstrated abnormal relaxation of the esophagogastric junction, abnormal relaxation median supine integrative relaxation pressure, hypertensive LES, no normal peristalsis with panesophageal pressurization in all swallows, scattered jackhammer activity and retrograde peristalsis and negligible upper esophageal sphincter tone. She underwent laparoscopic Heller esophagomyotomy for severe type 2 achalasia.
Discussion: Achalasia incidence rates were perceived lower until annual rates have risen to 1.6 per 100000 versus 0.5 - 1.2 per 100000. Achalasia appears to affect individuals by bimodal age distribution at diagnosis with the greatest incidence in the 3rd-4th decade and the other at 60 years of age, close to the median age of our patients with achalasia and WE. This case highlights WE as an atypical presentation of achalasia and outcomes despite aggressive management of late-stage disease.

Figure: A. Normal Clouse Plot (left) , B. Abnormal Clouse Plot (right) respective to our patient with type II achalasia demonstrating the presence of paraesophageal pressurization, absent normal peristalsis and elevation of integrated relaxation pressures.
Disclosures:
Diana Rodriguez indicated no relevant financial relationships.
Kriti Gera indicated no relevant financial relationships.
Vanessa Rodriguez indicated no relevant financial relationships.
Angela Pham indicated no relevant financial relationships.
Diana N. Rodriguez, MD1, Kriti Gera, MD1, Vanessa I. Rodriguez, MD2, Angela Pham, MD3. P1898 - A Case of Wernicke’s Encephalopathy Due to Type 2 Achalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
