Monday Poster Session
Category: Esophagus
P1904 - Inlet Patch Esophageal Stricture
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Jonathan Pham, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Jonathan Pham, MD, Nayantara Coelho-Prabhu, MBBS
Mayo Clinic, Rochester, MN
Introduction: Although inlet patches are common, they are typically asymptomatic and are usually incidental findings. Rarely, strictures can occur as a result of inlet patch acid production and may lead to dysphagia. We present a case of an inlet patch related esophageal stricture to highlight disease diagnosis and management.
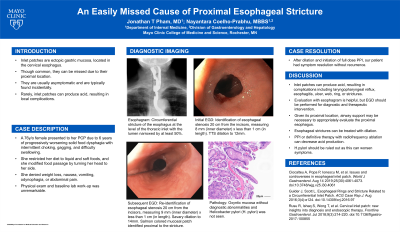
Case Description/Methods: A 76y/o female presented to her primary care provider after 6 years of intermittent, progressively worsening solid food dysphagia that would occur at least twice a month, resulting in a restricted diet. She had a fluoroscopic video swallow study with esophagram, which showed a circumferential stricture of the esophagus at the level of the thoracic inlet with the lumen narrowed by at least 50%. As part of her dysphagia investigation, she had an EGD that showed a stenosis 20cm from the incisor, measuring 8mm (inner diameter) x less than 1cm (in length). Her stenosis was dilated to 12mm, and she started on full dose PPI BID. She was scheduled for a repeat EGD 3 weeks later, which identified circumferential salmon-colored mucosa from 18cm to 20cm from the incisor with a stenosis at the lower margin. Her stenosis was dilated to 14mm. The esophageal biopsy showed oxyntic mucosa without diagnostic abnormalities and no H.pylori was seen. She had symptomatic improvement after PPI and dilation of her stricture.
Discussion: Inlet patch is ectopic gastric mucosa that occurs in the cervical esophagus, typically just distal to the upper esophageal sphincter. They are most commonly noted as an isolated patch. Most are asymptomatic; however, complications can occur due to acid secretion resulting in esophagitis, ulcer, web, or stricture formation. Dilation may be needed to relieve symptoms and radio frequency ablation has been attempted to decrease acid production at this site. Additionally, up to 82% of inlet patches are infected with H.pylori that may worsen esophageal symptoms. As in this case, an inlet patch can be overlooked due to its proximal location. A high clinical suspicion and careful evaluation including biopsies should be performed, especially in the setting of unexplained esophageal symptoms or endoscopic findings of inlet patch related complications.

Disclosures:
Jonathan Pham, MD, Nayantara Coelho-Prabhu, MBBS. P1904 - Inlet Patch Esophageal Stricture, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Although inlet patches are common, they are typically asymptomatic and are usually incidental findings. Rarely, strictures can occur as a result of inlet patch acid production and may lead to dysphagia. We present a case of an inlet patch related esophageal stricture to highlight disease diagnosis and management.
Case Description/Methods: A 76y/o female presented to her primary care provider after 6 years of intermittent, progressively worsening solid food dysphagia that would occur at least twice a month, resulting in a restricted diet. She had a fluoroscopic video swallow study with esophagram, which showed a circumferential stricture of the esophagus at the level of the thoracic inlet with the lumen narrowed by at least 50%. As part of her dysphagia investigation, she had an EGD that showed a stenosis 20cm from the incisor, measuring 8mm (inner diameter) x less than 1cm (in length). Her stenosis was dilated to 12mm, and she started on full dose PPI BID. She was scheduled for a repeat EGD 3 weeks later, which identified circumferential salmon-colored mucosa from 18cm to 20cm from the incisor with a stenosis at the lower margin. Her stenosis was dilated to 14mm. The esophageal biopsy showed oxyntic mucosa without diagnostic abnormalities and no H.pylori was seen. She had symptomatic improvement after PPI and dilation of her stricture.
Discussion: Inlet patch is ectopic gastric mucosa that occurs in the cervical esophagus, typically just distal to the upper esophageal sphincter. They are most commonly noted as an isolated patch. Most are asymptomatic; however, complications can occur due to acid secretion resulting in esophagitis, ulcer, web, or stricture formation. Dilation may be needed to relieve symptoms and radio frequency ablation has been attempted to decrease acid production at this site. Additionally, up to 82% of inlet patches are infected with H.pylori that may worsen esophageal symptoms. As in this case, an inlet patch can be overlooked due to its proximal location. A high clinical suspicion and careful evaluation including biopsies should be performed, especially in the setting of unexplained esophageal symptoms or endoscopic findings of inlet patch related complications.

Figure: Diagnostic studies for a patient with inlet patch esophageal stricture. (A) Esophagram showing a stricture at the level of the thoracic inlet. (B) Initial EGD without clear identification of the inlet patch. (C) Subsequent EGD showing distinct mucosal borders of the inlet patch. (D) Histology evaluation of the inlet patch biopsy showing oxyntic mucosa.
Disclosures:
Jonathan Pham indicated no relevant financial relationships.
Nayantara Coelho-Prabhu: Alexion Pharma – Advisor or Review Panel Member. Iterative Health – Advisor or Review Panel Member.
Jonathan Pham, MD, Nayantara Coelho-Prabhu, MBBS. P1904 - Inlet Patch Esophageal Stricture, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
