Monday Poster Session
Category: Esophagus
P1906 - Esophageal Hematoma After Transesophageal Echocardiogram: A Case Review
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- NC
Nicole Cornet, MD
New York-Presbyterian Hospital/Weill Cornell Medical College
New York, NY
Presenting Author(s)
Nicole Cornet, MD1, Lasha Gogokhia, MD2, David Wan, BS, MD3
1New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Esophageal hematoma (EH) is a rare cause of submucosal bleeding, and may be spontaneous or secondary to foreign body trauma, toxic or sharp ingestion, or iatrogenic intervention. Risk factors include increased age, use of anticoagulation (AC) or antithrombotic agents, and frequent endoscopic instrumentation. EH portends a favorable prognosis, though complications may arise if not identified early.
Case Description/Methods: A 78-year-old female with prior lower gastrointestinal bleed and atrial fibrillation (not on AC) presented for uncomplicated transesophageal echocardiogram (TEE)-guided left atrial appendage occlusion (LAAO) insertion. In post-op, she developed acute-onset chest pain and hypotension that was responsive to fluids. Cardiac workup was unremarkable. CT chest showed esophageal distention with long segment EH and no evidence of mediastinal hematoma or pneumomediastinum. Given hemodynamic stability and lack of hematemesis, she was managed conservatively with intravenous (IV) fluids, high dose IV proton pump inhibitor (PPI), and NPO. Over the next 24 hours, she remained hemodynamically stable and was tolerating a regular diet with resolution of the chest pain. Follow up CT scan two weeks later demonstrated resolution of the EH, and she was successfully started on aspirin without further bleeding or chest pain.
Discussion: The triad of EH includes acute chest pain, hematemesis, and dysphagia. Once cardiac etiologies are ruled out, the standard for diagnosis is CT chest revealing an intra-esophageal mass or filling defect, thickened esophageal wall, and luminal compression or obliteration in severe cases. Endoscopy should be deferred until the esophageal wall integrity has been preserved, though may be done sooner if CT findings are equivocal or indicative of rupture. In cases with hemodynamic stability, treatment is conservative with serial CT images to assess for resolution of the hematoma in one to two weeks. In severe cases, such as those with hemodynamic instability, failure to respond to conservative measures, or esophageal obstruction or perforation, emergent endoscopy or surgery may be indicated. Endoscopy reveals a red-purplish raised lesion of varying size, often submucosal though may obstruct the esophageal lumen. Overall, it is important to handle an endoscope gently, especially in patients with risk factors for EH, and to consider EH in a patient with acute onset chest pain and evidence of gastrointestinal bleed or discomfort following intra-esophageal instrumentation.

Disclosures:
Nicole Cornet, MD1, Lasha Gogokhia, MD2, David Wan, BS, MD3. P1906 - Esophageal Hematoma After Transesophageal Echocardiogram: A Case Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Esophageal hematoma (EH) is a rare cause of submucosal bleeding, and may be spontaneous or secondary to foreign body trauma, toxic or sharp ingestion, or iatrogenic intervention. Risk factors include increased age, use of anticoagulation (AC) or antithrombotic agents, and frequent endoscopic instrumentation. EH portends a favorable prognosis, though complications may arise if not identified early.
Case Description/Methods: A 78-year-old female with prior lower gastrointestinal bleed and atrial fibrillation (not on AC) presented for uncomplicated transesophageal echocardiogram (TEE)-guided left atrial appendage occlusion (LAAO) insertion. In post-op, she developed acute-onset chest pain and hypotension that was responsive to fluids. Cardiac workup was unremarkable. CT chest showed esophageal distention with long segment EH and no evidence of mediastinal hematoma or pneumomediastinum. Given hemodynamic stability and lack of hematemesis, she was managed conservatively with intravenous (IV) fluids, high dose IV proton pump inhibitor (PPI), and NPO. Over the next 24 hours, she remained hemodynamically stable and was tolerating a regular diet with resolution of the chest pain. Follow up CT scan two weeks later demonstrated resolution of the EH, and she was successfully started on aspirin without further bleeding or chest pain.
Discussion: The triad of EH includes acute chest pain, hematemesis, and dysphagia. Once cardiac etiologies are ruled out, the standard for diagnosis is CT chest revealing an intra-esophageal mass or filling defect, thickened esophageal wall, and luminal compression or obliteration in severe cases. Endoscopy should be deferred until the esophageal wall integrity has been preserved, though may be done sooner if CT findings are equivocal or indicative of rupture. In cases with hemodynamic stability, treatment is conservative with serial CT images to assess for resolution of the hematoma in one to two weeks. In severe cases, such as those with hemodynamic instability, failure to respond to conservative measures, or esophageal obstruction or perforation, emergent endoscopy or surgery may be indicated. Endoscopy reveals a red-purplish raised lesion of varying size, often submucosal though may obstruct the esophageal lumen. Overall, it is important to handle an endoscope gently, especially in patients with risk factors for EH, and to consider EH in a patient with acute onset chest pain and evidence of gastrointestinal bleed or discomfort following intra-esophageal instrumentation.

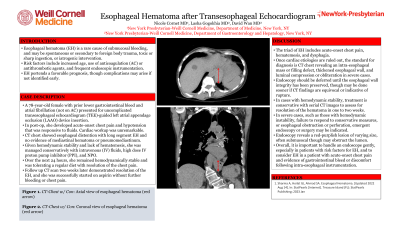
Figure: CT chest showing esophageal hematoma (red arrow) in the axial and coronal planes
Disclosures:
Nicole Cornet indicated no relevant financial relationships.
Lasha Gogokhia indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Nicole Cornet, MD1, Lasha Gogokhia, MD2, David Wan, BS, MD3. P1906 - Esophageal Hematoma After Transesophageal Echocardiogram: A Case Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
