Monday Poster Session
Category: Esophagus
P1911 - Unveiling the Link: SVC Thrombosis and the Emergence of Esophageal Varices
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Petro Shafranyuk, MD
Franciscan Health Olympia Fields
Olympia Fields, IL
Presenting Author(s)
Petro Shafranyuk, MD1, Saria Adnan Sultan, DO2, Sana Saleem, MD2, Shana Kothari, MD3, Alex Yarbrough, DO1
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Franciscan Health, Chicago, IL; 3Franciscan Health, Olympia Fields, IL
Introduction: Proximal esophageal varices also termed downhill varices represent a small subset of esophageal varices of around 0.4-10%. They often form due to venous hypertension of the superior systemic circulation most often from superior vena cava (SVC) obstruction. The most common cause of SVC obstruction is malignancy, however other causes include vascular phenomenon involving systemic vasculitis or trauma, presence of an intravascular device, and fibrosing mediastinitis. SVC obstruction should be corrected, especially in patients who are at high risk of bleeding. Our case presents a patient with an incidental finding of proximal esophageal varices on upper endoscopy after investigation for an upper gastrointestinal bleed. This prompted further imaging showing SVC obstruction likely from a previous central venous catheter line placement.
Case Description/Methods: A 47 year old male with bilateral paraplegia secondary to gunshot wound and colostomy bag due to chronic coccyx decubitus ulcers presented with 2 weeks of progressively worsening diarrhea and hematemesis. Initial labs were significant for BUN 52mg/dL, Cr 1.0mg/dL, and Hgb 7.2 g/dL. Patient underwent endoscopy, which showed one actively bleeding cratered gastric ulcer (Forest Class 1b) and incidental grade I varices in the proximal and mid esophagus. Due to proximal esophageal varices a CT chest was ordered, which showed SVC occlusion. Further investigation revealed that the patient had multiple peripherally inserted central catheter (PICC) line placements and port-a-cath in the past. Patient remained hemodynamically stable, and was discharged with follow up with interventional radiology for management of SVC obstruction.
Discussion: It is crucial to remember that the frequent utilization of central venous catheters, PICC lines, and port-a-catheters escalates the risk of complications, notably SVC obstruction. This condition can subsequently develop proximal esophageal varices, which can pose a life-threatening risk of severe upper gastrointestinal bleeding. Treatment of proximal esophageal varices poses many risks given its location. Unfortunately, there is a lack of established protocols for screening or managing SVC obstruction and upper esophageal varices. However, it is important for healthcare providers to keep a close watch on patients who have had multiple central venous catheters and PICC lines in the past. Management should be directed in treating the underlying cause of obstruction and prevent varices formation.

Disclosures:
Petro Shafranyuk, MD1, Saria Adnan Sultan, DO2, Sana Saleem, MD2, Shana Kothari, MD3, Alex Yarbrough, DO1. P1911 - Unveiling the Link: SVC Thrombosis and the Emergence of Esophageal Varices, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Franciscan Health, Chicago, IL; 3Franciscan Health, Olympia Fields, IL
Introduction: Proximal esophageal varices also termed downhill varices represent a small subset of esophageal varices of around 0.4-10%. They often form due to venous hypertension of the superior systemic circulation most often from superior vena cava (SVC) obstruction. The most common cause of SVC obstruction is malignancy, however other causes include vascular phenomenon involving systemic vasculitis or trauma, presence of an intravascular device, and fibrosing mediastinitis. SVC obstruction should be corrected, especially in patients who are at high risk of bleeding. Our case presents a patient with an incidental finding of proximal esophageal varices on upper endoscopy after investigation for an upper gastrointestinal bleed. This prompted further imaging showing SVC obstruction likely from a previous central venous catheter line placement.
Case Description/Methods: A 47 year old male with bilateral paraplegia secondary to gunshot wound and colostomy bag due to chronic coccyx decubitus ulcers presented with 2 weeks of progressively worsening diarrhea and hematemesis. Initial labs were significant for BUN 52mg/dL, Cr 1.0mg/dL, and Hgb 7.2 g/dL. Patient underwent endoscopy, which showed one actively bleeding cratered gastric ulcer (Forest Class 1b) and incidental grade I varices in the proximal and mid esophagus. Due to proximal esophageal varices a CT chest was ordered, which showed SVC occlusion. Further investigation revealed that the patient had multiple peripherally inserted central catheter (PICC) line placements and port-a-cath in the past. Patient remained hemodynamically stable, and was discharged with follow up with interventional radiology for management of SVC obstruction.
Discussion: It is crucial to remember that the frequent utilization of central venous catheters, PICC lines, and port-a-catheters escalates the risk of complications, notably SVC obstruction. This condition can subsequently develop proximal esophageal varices, which can pose a life-threatening risk of severe upper gastrointestinal bleeding. Treatment of proximal esophageal varices poses many risks given its location. Unfortunately, there is a lack of established protocols for screening or managing SVC obstruction and upper esophageal varices. However, it is important for healthcare providers to keep a close watch on patients who have had multiple central venous catheters and PICC lines in the past. Management should be directed in treating the underlying cause of obstruction and prevent varices formation.

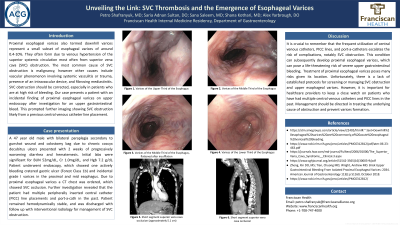
Figure: Image A. Endoscopic imaging showing the upper third of esophagus with grade I esophageal varices
Image B. Endoscopic imaging showing the middle third of esophagus with grade I esophageal varices
Image C. CT Chest W Contrast showing short segment SVC occlusion (approximately 5.1 cm)
Image B. Endoscopic imaging showing the middle third of esophagus with grade I esophageal varices
Image C. CT Chest W Contrast showing short segment SVC occlusion (approximately 5.1 cm)
Disclosures:
Petro Shafranyuk indicated no relevant financial relationships.
Saria Adnan Sultan indicated no relevant financial relationships.
Sana Saleem indicated no relevant financial relationships.
Shana Kothari indicated no relevant financial relationships.
Alex Yarbrough indicated no relevant financial relationships.
Petro Shafranyuk, MD1, Saria Adnan Sultan, DO2, Sana Saleem, MD2, Shana Kothari, MD3, Alex Yarbrough, DO1. P1911 - Unveiling the Link: SVC Thrombosis and the Emergence of Esophageal Varices, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
