Monday Poster Session
Category: Colon
P1727 - Eosinophilic Colitis in a Patient With Seronegative Rheumatoid Arthritis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Mohsen Dourra, MD
Corewell Health
Woodhaven, MI
Presenting Author(s)
Mohsen Dourra, MD1, Rukmini Enjamuri, MD2, Olga Brushaber, DO3, John C. Pui, MD4
1Corewell Health, Woodhaven, MI; 2Beaumont, Porter Ranch, CA; 3Corewell Health, Farmington, MI; 4Corewell Health East, Farmington Hills, MI
Introduction: Eosinophilic colitis (EoC) is the rarest eosinophilic gastrointestinal disease (EGID) with an overall prevalence of 2.1 per 100,000 subjects. EoC can be difficult to diagnose given the diverse symptomatology and high clinical suspicion required for recognition. In addition, association with autoimmune disease is seldom reported. Here, we discuss a unique case of EoC in a patient with seronegative rheumatoid arthritis (RA).
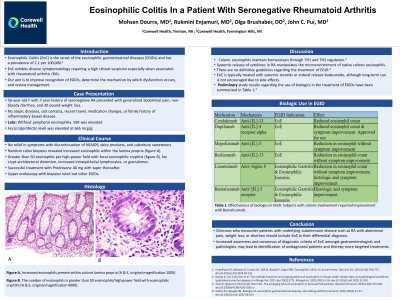
Case Description/Methods: A 56-year-old female with a seven-year history of seronegative RA presented with generalized abdominal pain, non-bloody diarrhea, and 30-pound weight loss. The patient denied a history of atopic diseases, sick contact, recent travel, medication changes, or family history of inflammatory bowel disease. She had been treated with methotrexate, leflunomide, and hydroxychloroquine with good tolerance. Workup included an elevated calprotectin level of 665 and normal stool studies. Colonoscopy revealed endoscopically normal colon. Random colon biopsies revealed increased eosinophils within the lamina propria (figure A). The number of eosinophils ranged up to greater than 50 eosinophils per high-power field with focal eosinophilic cryptitis (figure B). She did not have relief in symptoms with discontinuation of non-steroidal anti-inflammatory drugs, dairy products, and substitute sweeteners. Patient was ultimately diagnosed with EoC and given a trial of prednisone taper with improvement in symptoms.
Discussion: The pathogenesis of RA induced EoC is hypothesized to involve the link between atopy and autoimmunity, referring to Th1/Th2 modulation. Chemoattractants, such as eotaxin, IL-5, and MCP-4, released by innate lymphoid cells and Th2 cells contribute to EoC pathogenesis. Treatment with systemic steroids can be associated with adverse effects and symptom recurrence, highlighting the importance of steroid-sparing medications. Immunomodulatory agents (azathioprine, 6-mercaptpurine) and anti-TNF agents (infliximab, adalimumab) have been tried in severe, steroid-refractory EoC with promising results. Targeted therapy in the form of biologics are still being studied in the treatment of EGID. Clinicians who encounter patients with underlying autoimmune disease with altered bowel habits, weight loss, or abdominal pain should include EoC in their differential diagnosis. Increased awareness and consensus of diagnostic criteria of EoC may lead to identification of undiagnosed patients and thereby more targeted treatments.

Disclosures:
Mohsen Dourra, MD1, Rukmini Enjamuri, MD2, Olga Brushaber, DO3, John C. Pui, MD4. P1727 - Eosinophilic Colitis in a Patient With Seronegative Rheumatoid Arthritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Corewell Health, Woodhaven, MI; 2Beaumont, Porter Ranch, CA; 3Corewell Health, Farmington, MI; 4Corewell Health East, Farmington Hills, MI
Introduction: Eosinophilic colitis (EoC) is the rarest eosinophilic gastrointestinal disease (EGID) with an overall prevalence of 2.1 per 100,000 subjects. EoC can be difficult to diagnose given the diverse symptomatology and high clinical suspicion required for recognition. In addition, association with autoimmune disease is seldom reported. Here, we discuss a unique case of EoC in a patient with seronegative rheumatoid arthritis (RA).
Case Description/Methods: A 56-year-old female with a seven-year history of seronegative RA presented with generalized abdominal pain, non-bloody diarrhea, and 30-pound weight loss. The patient denied a history of atopic diseases, sick contact, recent travel, medication changes, or family history of inflammatory bowel disease. She had been treated with methotrexate, leflunomide, and hydroxychloroquine with good tolerance. Workup included an elevated calprotectin level of 665 and normal stool studies. Colonoscopy revealed endoscopically normal colon. Random colon biopsies revealed increased eosinophils within the lamina propria (figure A). The number of eosinophils ranged up to greater than 50 eosinophils per high-power field with focal eosinophilic cryptitis (figure B). She did not have relief in symptoms with discontinuation of non-steroidal anti-inflammatory drugs, dairy products, and substitute sweeteners. Patient was ultimately diagnosed with EoC and given a trial of prednisone taper with improvement in symptoms.
Discussion: The pathogenesis of RA induced EoC is hypothesized to involve the link between atopy and autoimmunity, referring to Th1/Th2 modulation. Chemoattractants, such as eotaxin, IL-5, and MCP-4, released by innate lymphoid cells and Th2 cells contribute to EoC pathogenesis. Treatment with systemic steroids can be associated with adverse effects and symptom recurrence, highlighting the importance of steroid-sparing medications. Immunomodulatory agents (azathioprine, 6-mercaptpurine) and anti-TNF agents (infliximab, adalimumab) have been tried in severe, steroid-refractory EoC with promising results. Targeted therapy in the form of biologics are still being studied in the treatment of EGID. Clinicians who encounter patients with underlying autoimmune disease with altered bowel habits, weight loss, or abdominal pain should include EoC in their differential diagnosis. Increased awareness and consensus of diagnostic criteria of EoC may lead to identification of undiagnosed patients and thereby more targeted treatments.

Figure: A: Increased eosinophils present within colonic lamina propria (H & E, original magnification 100X).
B: The number of eosinophils is greater than 50 eosinophils/high power field with eosinophilic cryptitis (H & E, original magnification 400X).
B: The number of eosinophils is greater than 50 eosinophils/high power field with eosinophilic cryptitis (H & E, original magnification 400X).
Disclosures:
Mohsen Dourra indicated no relevant financial relationships.
Rukmini Enjamuri indicated no relevant financial relationships.
Olga Brushaber indicated no relevant financial relationships.
John Pui indicated no relevant financial relationships.
Mohsen Dourra, MD1, Rukmini Enjamuri, MD2, Olga Brushaber, DO3, John C. Pui, MD4. P1727 - Eosinophilic Colitis in a Patient With Seronegative Rheumatoid Arthritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
