Monday Poster Session
Category: Biliary/Pancreas
P1498 - A Jejunal Artery Pseudoaneurysm Rupture into Pancreatic Pseudocyst: A Case Report
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Sharifeh Almasaid, MD
SUNY Upstate University Hospital
Syracuse, NY
Presenting Author(s)
Sharifeh Almasaid, MD1, Fathima Keshia Suhail, MD2, Hatem al Kashroom, MBBS1, Hafiz M. Khan, MD2, Ganesh Aswath, MD3
1SUNY Upstate University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Upstate University Hospital, Syracuse, NY
Introduction: Chronic pancreatitis has fibroinflammatory episodes that irreversibly affect pancreatic parenchyma, resulting in both morphological and functional alterations. Among the various complications it has, the formation of pseudocysts is notable and in some cases, bleeding into the pseudocyst is a possibility. In this report we present a case of chronic pancreatitis with pancreatic pseudocyst eroding into one of superior mesenteric artery (SMA) branches, causing significant bleeding.
Case Description/Methods: A 58-year-old Caucasian female with a history of chronic pancreatitis complicated by enlarging pseudocyst, came with a sudden onset of severe abdominal pain radiating to her back, with diffuse tenderness on exam. Prior to presentation, she had MRI that showed a large pancreatic head pseudocyst displacing the SMA inferiorly, with a subtle pseudoaneurysm seen at the first jejunal branch. Repeat imaging on admission demonstrated a large pancreatic pseudocyst with an area of active extravasation of contrast within the pseudocyst.
She underwent evaluation by surgical and interventional radiology (IR) teams, leading to the performance of an arteriogram of the SMA. It revealed a pseudoaneurysm originating from the Jejunal branch of the SMA with an active extravasation into the pseudocyst. The condition was managed through coil embolization, which stabilized the patient and stopped the bleeding.
Discussion: Pancreatic pseudocysts can be seen in chronic pancreatitis. Formed pseudoaneurysms commonly affect the splenic artery, followed by the gastroduodenal artery, with only a limited number of reported cases involving the SMA in chronic pancreatitis. SMA pseudoaneurysms account for 6-8% of all visceral arterial pseudoaneurysms, making them exceptionally rare with an occurrence rate of 0.01%. The occurrence of visceral vessel rupture and subsequent bleeding into the pseudocyst is even rarer. Despite their rarity, they pose a significant risk for bowel ischemia and potential mortality. IR approaches are preferred for addressing the bleeding, as it offers a high success rate and reduced risk. If unsuccessful, surgical options may be considered.
Our case stands out as the second reported occurrence of SMA Jejunal branch involvement in the literature, highlighting its uniqueness. Despite the subtle bleeding, it led to a significant hemorrhage, underscoring the importance of timely intervention upon imaging detection and collaborative planning among interdisciplinary teams.

Disclosures:
Sharifeh Almasaid, MD1, Fathima Keshia Suhail, MD2, Hatem al Kashroom, MBBS1, Hafiz M. Khan, MD2, Ganesh Aswath, MD3. P1498 - A Jejunal Artery Pseudoaneurysm Rupture into Pancreatic Pseudocyst: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SUNY Upstate University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Upstate University Hospital, Syracuse, NY
Introduction: Chronic pancreatitis has fibroinflammatory episodes that irreversibly affect pancreatic parenchyma, resulting in both morphological and functional alterations. Among the various complications it has, the formation of pseudocysts is notable and in some cases, bleeding into the pseudocyst is a possibility. In this report we present a case of chronic pancreatitis with pancreatic pseudocyst eroding into one of superior mesenteric artery (SMA) branches, causing significant bleeding.
Case Description/Methods: A 58-year-old Caucasian female with a history of chronic pancreatitis complicated by enlarging pseudocyst, came with a sudden onset of severe abdominal pain radiating to her back, with diffuse tenderness on exam. Prior to presentation, she had MRI that showed a large pancreatic head pseudocyst displacing the SMA inferiorly, with a subtle pseudoaneurysm seen at the first jejunal branch. Repeat imaging on admission demonstrated a large pancreatic pseudocyst with an area of active extravasation of contrast within the pseudocyst.
She underwent evaluation by surgical and interventional radiology (IR) teams, leading to the performance of an arteriogram of the SMA. It revealed a pseudoaneurysm originating from the Jejunal branch of the SMA with an active extravasation into the pseudocyst. The condition was managed through coil embolization, which stabilized the patient and stopped the bleeding.
Discussion: Pancreatic pseudocysts can be seen in chronic pancreatitis. Formed pseudoaneurysms commonly affect the splenic artery, followed by the gastroduodenal artery, with only a limited number of reported cases involving the SMA in chronic pancreatitis. SMA pseudoaneurysms account for 6-8% of all visceral arterial pseudoaneurysms, making them exceptionally rare with an occurrence rate of 0.01%. The occurrence of visceral vessel rupture and subsequent bleeding into the pseudocyst is even rarer. Despite their rarity, they pose a significant risk for bowel ischemia and potential mortality. IR approaches are preferred for addressing the bleeding, as it offers a high success rate and reduced risk. If unsuccessful, surgical options may be considered.
Our case stands out as the second reported occurrence of SMA Jejunal branch involvement in the literature, highlighting its uniqueness. Despite the subtle bleeding, it led to a significant hemorrhage, underscoring the importance of timely intervention upon imaging detection and collaborative planning among interdisciplinary teams.

Figure: Figure [1]
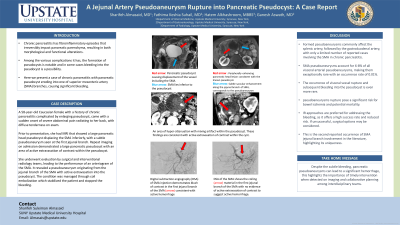
Image (A): Coronal T2 weighted image demonstrate large T2 hyperintense pancreatic pseudocyst that causing displacement of the vessels including the SMA; which lies inferior to the pseudocyst (arrowhead)
Image (B): Axial contrast enhanced (arterial phase) T1 weight image shows a peripherally enhancing pancreatic head lesion consistent with the known pseudocyst. The arrowhead shows a subtle saccular enhancement along the jejunal branch of SMA, which corresponds to the pseudoaneurysm.
Figure [2]
Image (A): Axial contrast enhanced CT abdomen (portal venous phase) shows an area of hyper-attenuation with mixing artifact of the within the pseudocyst. These findings are consistent with active extravasation of contrast within the cyst.
Image (B): Sagittal contrast enhanced CT abdomen (portal venous phase) shows an area of hyper-attenuation with mixing artifact of the within the pseudocyst. These findings are consistent with active extravasation of contrast within the cyst.
Figure [3]
Image (A): Digital subtraction angiography (DSA) of SMA injection demonstrates blush of contrast in the first jejunal branch of the SMA (arrow) consistent with active hemorrhage.
Image (B): DSA of the SMA shows the coiling material in the first jejunal branch of the SMA with no evidence of active extravasation of contrast to suggest active hemorrhage
Image (A): Coronal T2 weighted image demonstrate large T2 hyperintense pancreatic pseudocyst that causing displacement of the vessels including the SMA; which lies inferior to the pseudocyst (arrowhead)
Image (B): Axial contrast enhanced (arterial phase) T1 weight image shows a peripherally enhancing pancreatic head lesion consistent with the known pseudocyst. The arrowhead shows a subtle saccular enhancement along the jejunal branch of SMA, which corresponds to the pseudoaneurysm.
Figure [2]
Image (A): Axial contrast enhanced CT abdomen (portal venous phase) shows an area of hyper-attenuation with mixing artifact of the within the pseudocyst. These findings are consistent with active extravasation of contrast within the cyst.
Image (B): Sagittal contrast enhanced CT abdomen (portal venous phase) shows an area of hyper-attenuation with mixing artifact of the within the pseudocyst. These findings are consistent with active extravasation of contrast within the cyst.
Figure [3]
Image (A): Digital subtraction angiography (DSA) of SMA injection demonstrates blush of contrast in the first jejunal branch of the SMA (arrow) consistent with active hemorrhage.
Image (B): DSA of the SMA shows the coiling material in the first jejunal branch of the SMA with no evidence of active extravasation of contrast to suggest active hemorrhage
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Fathima Keshia Suhail indicated no relevant financial relationships.
Hatem al Kashroom indicated no relevant financial relationships.
Hafiz Khan indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Sharifeh Almasaid, MD1, Fathima Keshia Suhail, MD2, Hatem al Kashroom, MBBS1, Hafiz M. Khan, MD2, Ganesh Aswath, MD3. P1498 - A Jejunal Artery Pseudoaneurysm Rupture into Pancreatic Pseudocyst: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
