Monday Poster Session
Category: Biliary/Pancreas
P1499 - A Case of Breast Cancer Metastasizing to the Ampulla of Vater
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MT
Matthew Tjahja, MD, MS
Baylor Scott & White
Temple, TX
Presenting Author(s)
Matthew Tjahja, MD, MS, Phi Tran, DO, Jonathan Ramirez, MD
Baylor Scott & White, Temple, TX
Introduction: We present a 72-year-old patient who was found to have ampullary metastasis from breast carcinoma despite treatment with radical mastectomy 27 years prior and chemotherapy, which was stopped in 2000.
Case Description/Methods: A 72-year-old female with PMH of breast cancer with bilateral mastectomy and chemo, HTN, HLD, and OA presented with altered mental status and was found to have elevated LFTs with T bili 4.0, ALP 787, AST 1454, ALT 1342, and ammonia 61. CT Abdomenn was concerning for multiple liver lesions of unknown etiology, and a distended gallbladder with CBD 8mm, but no stones.
The patient underwent EGD/EUS revealing an edematous and erythematous periampullary region and moderate non-erosive gastritis. Pathology revealed intestinal mucosa focally involved by carcinoma that was positive for pankeratin (AE1/AE3) and CD138, and negative for CD45 and S100 supporting the diagnosis of metastatic breast carcinoma
PET scan revealed areas of increased tracer activity including multiple ribs/vertebrae, and bones within her extremities. Due to the extent of metastatic disease and lack of persistent cholestasis, an ampullectomy/sphincterotomy was not performed. She has been treated with palliative chemo and continues to undergo regular surveillance with no evidence of progression.
Discussion: Metastasis of any type to the ampulla can present as upper GI bleeding, jaundice, nausea, and vomiting. Our patient presented with altered mental status and was found to have elevated LFTs. The average time from diagnosis of breast cancer to metastasis to the ampulla was found to be 2.5 years. Our patient’s initial diagnosis of breast cancer was roughly 27 years prior. However, it should be noted that roughly 4 years ago, the patient was found to have a mass on mammogram, which was subsequently removed. Thus, the argument could be made that this metastasis was roughly 4 years from a second diagnosis of breast cancer. Primary and secondary cancers cannot be visually distinguished so definitive diagnosis requires biopsy with cytology and immunohistochemical analysis.
In conclusion, metastatic cancer to the ampulla of Vater is a rare occurrence that most frequently occurs with renal cell carcinoma and malignant skin melanoma primaries. Secondary breast cancer is relatively rare. Biopsy with cytology and immunohistochemistry is needed to distinguish primary vs secondary tumors. Treatment is usually palliative, but can include any combination of surgery, chemotherapy, and ampullectomy.

Disclosures:
Matthew Tjahja, MD, MS, Phi Tran, DO, Jonathan Ramirez, MD. P1499 - A Case of Breast Cancer Metastasizing to the Ampulla of Vater, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Baylor Scott & White, Temple, TX
Introduction: We present a 72-year-old patient who was found to have ampullary metastasis from breast carcinoma despite treatment with radical mastectomy 27 years prior and chemotherapy, which was stopped in 2000.
Case Description/Methods: A 72-year-old female with PMH of breast cancer with bilateral mastectomy and chemo, HTN, HLD, and OA presented with altered mental status and was found to have elevated LFTs with T bili 4.0, ALP 787, AST 1454, ALT 1342, and ammonia 61. CT Abdomenn was concerning for multiple liver lesions of unknown etiology, and a distended gallbladder with CBD 8mm, but no stones.
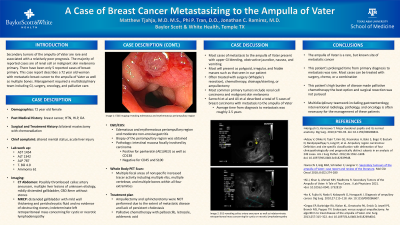
The patient underwent EGD/EUS revealing an edematous and erythematous periampullary region and moderate non-erosive gastritis. Pathology revealed intestinal mucosa focally involved by carcinoma that was positive for pankeratin (AE1/AE3) and CD138, and negative for CD45 and S100 supporting the diagnosis of metastatic breast carcinoma
PET scan revealed areas of increased tracer activity including multiple ribs/vertebrae, and bones within her extremities. Due to the extent of metastatic disease and lack of persistent cholestasis, an ampullectomy/sphincterotomy was not performed. She has been treated with palliative chemo and continues to undergo regular surveillance with no evidence of progression.
Discussion: Metastasis of any type to the ampulla can present as upper GI bleeding, jaundice, nausea, and vomiting. Our patient presented with altered mental status and was found to have elevated LFTs. The average time from diagnosis of breast cancer to metastasis to the ampulla was found to be 2.5 years. Our patient’s initial diagnosis of breast cancer was roughly 27 years prior. However, it should be noted that roughly 4 years ago, the patient was found to have a mass on mammogram, which was subsequently removed. Thus, the argument could be made that this metastasis was roughly 4 years from a second diagnosis of breast cancer. Primary and secondary cancers cannot be visually distinguished so definitive diagnosis requires biopsy with cytology and immunohistochemical analysis.
In conclusion, metastatic cancer to the ampulla of Vater is a rare occurrence that most frequently occurs with renal cell carcinoma and malignant skin melanoma primaries. Secondary breast cancer is relatively rare. Biopsy with cytology and immunohistochemistry is needed to distinguish primary vs secondary tumors. Treatment is usually palliative, but can include any combination of surgery, chemotherapy, and ampullectomy.

Figure: Endoscopic visualization of ampullary carcinoma and EUS imaging demonstrating incidental celiac artery aneurysm
Disclosures:
Matthew Tjahja indicated no relevant financial relationships.
Phi Tran indicated no relevant financial relationships.
Jonathan Ramirez indicated no relevant financial relationships.
Matthew Tjahja, MD, MS, Phi Tran, DO, Jonathan Ramirez, MD. P1499 - A Case of Breast Cancer Metastasizing to the Ampulla of Vater, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
