Tuesday Poster Session
Category: IBD
P3647 - Performance of ASCVD Risk Prediction Models in Individuals with Inflammatory Bowel Disease: A UK Biobank Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Quazim Alayo, MD, MSc, MMSc
Washington University School of Medicine
St. Louis, MO
Presenting Author(s)
Quazim Alayo, MD, MSc, MMSc1, Daniel Famutimi, MBBS, MPH2, Malek Ayoub, MD1, Parakkal Deepak, MBBS, MS3
1Washington University School of Medicine, St. Louis, MO; 2University of Missouri Health Care, Columbia, MO; 3Washington University in St. Louis School of Medicine, St. Louis, MO
Introduction: Individuals with inflammatory bowel disease (IBD) have been shown to have a higher risk of atherosclerotic cardiovascular disease (ASCVD) compared to the general population. However, the performance of the European Society of Cardiology (ESC) Systematic Coronary Risk Evaluation 2 (SCORE2) and the 2018 ACC/AHA Pooled Cohort Equations (PCE) has not been extensively studied in patients with IBD. This study aims to compare the performance of two different ASCVD risk prediction models in IBD and non-IBD cohorts using the UK Biobank study (UKB).
Methods: Using a validated selection process, we identified participants with IBD and ASCVD in the UKB study. Incident ASCVD was defined as a composite of non-fatal myocardial infarction, non-fatal stroke, and cardiovascular death occurring within 10 years of follow-up. The incidence rate of ASCVD events and incidence rate ratios were calculated. Receiver Operating Characteristic Area Under the Curve (ROC-AUC) for two models (ESC SCORE2 and ACC/AHA PCE) in IBD and non-IBD cohorts were calculated and compared using a two-sample t-test statistic. A sensitivity analysis was performed comparing IBD participants to age- and sex-matched non-IBD participants at a ratio of 1:4.
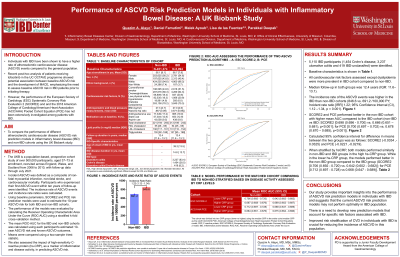
Results: 5110 IBD (3,237 UC, 1454 CD, 419 UC/CD) and 451,374 non-IBD participants were included in the sample. All cardiovascular risk factors assessed except dyslipidemia were more prevalent in IBD cohort compared to non-IBD (Table 1). After a median follow-up in either group of 12.4 years (IQR: 11.6–13.1), the incidence rate of ASCVD events (per 100,000 person-years) was higher among participants with IBD compared to participants without IBD (846.6 vs. 691.2 /100,000 PY; Incident rate ratio [IRR] 1.22; 95% Confidence Interval (CI), 1.12 –1.34, p = 0.001). Using the full study cohort, both risk prediction models performed better in the non-IBD cohort with higher mean AUC compared to the IBD cohort (SCORE2 [Non-IBD: 0.698 (0.696 - 0.700) vs. IBD: 0.666 (0.651 – 0.681), p< 0.001]; for PCE [Non-IBD: 0.700 (0.697 – 0.702) vs. IBD: 0.678 (0.670 – 0.685), p< 0.001]) (Figures 1A-1B). Similar findings were obtained in the sensitivity analysis when the IBD participants were compared to age- and sex-matched non-IBD participants (Figures 1C-1D).
Discussion: The current ASCVD risk prediction models in clinical practice do not perform optimally in individuals with IBD, and a better risk prediction model that accounts for IBD-specific risk factors may be needed for the IBD population.

Disclosures:
Quazim Alayo, MD, MSc, MMSc1, Daniel Famutimi, MBBS, MPH2, Malek Ayoub, MD1, Parakkal Deepak, MBBS, MS3. P3647 - Performance of ASCVD Risk Prediction Models in Individuals with Inflammatory Bowel Disease: A UK Biobank Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Washington University School of Medicine, St. Louis, MO; 2University of Missouri Health Care, Columbia, MO; 3Washington University in St. Louis School of Medicine, St. Louis, MO
Introduction: Individuals with inflammatory bowel disease (IBD) have been shown to have a higher risk of atherosclerotic cardiovascular disease (ASCVD) compared to the general population. However, the performance of the European Society of Cardiology (ESC) Systematic Coronary Risk Evaluation 2 (SCORE2) and the 2018 ACC/AHA Pooled Cohort Equations (PCE) has not been extensively studied in patients with IBD. This study aims to compare the performance of two different ASCVD risk prediction models in IBD and non-IBD cohorts using the UK Biobank study (UKB).
Methods: Using a validated selection process, we identified participants with IBD and ASCVD in the UKB study. Incident ASCVD was defined as a composite of non-fatal myocardial infarction, non-fatal stroke, and cardiovascular death occurring within 10 years of follow-up. The incidence rate of ASCVD events and incidence rate ratios were calculated. Receiver Operating Characteristic Area Under the Curve (ROC-AUC) for two models (ESC SCORE2 and ACC/AHA PCE) in IBD and non-IBD cohorts were calculated and compared using a two-sample t-test statistic. A sensitivity analysis was performed comparing IBD participants to age- and sex-matched non-IBD participants at a ratio of 1:4.
Results: 5110 IBD (3,237 UC, 1454 CD, 419 UC/CD) and 451,374 non-IBD participants were included in the sample. All cardiovascular risk factors assessed except dyslipidemia were more prevalent in IBD cohort compared to non-IBD (Table 1). After a median follow-up in either group of 12.4 years (IQR: 11.6–13.1), the incidence rate of ASCVD events (per 100,000 person-years) was higher among participants with IBD compared to participants without IBD (846.6 vs. 691.2 /100,000 PY; Incident rate ratio [IRR] 1.22; 95% Confidence Interval (CI), 1.12 –1.34, p = 0.001). Using the full study cohort, both risk prediction models performed better in the non-IBD cohort with higher mean AUC compared to the IBD cohort (SCORE2 [Non-IBD: 0.698 (0.696 - 0.700) vs. IBD: 0.666 (0.651 – 0.681), p< 0.001]; for PCE [Non-IBD: 0.700 (0.697 – 0.702) vs. IBD: 0.678 (0.670 – 0.685), p< 0.001]) (Figures 1A-1B). Similar findings were obtained in the sensitivity analysis when the IBD participants were compared to age- and sex-matched non-IBD participants (Figures 1C-1D).
Discussion: The current ASCVD risk prediction models in clinical practice do not perform optimally in individuals with IBD, and a better risk prediction model that accounts for IBD-specific risk factors may be needed for the IBD population.

Figure: Figure 1: ROC-AUC, Receiver Operating Characteristic Area Under the Curve assessing the performance of different ASCVD risk prediction algorithms in IBD and non-IBD cohort, A-B) ESC SCORE-2, European Society of Cardiology (ESC) Systematic Coronary Risk Evaluation 2 model (A and C), and ACC/AHA PCE, American College of Cardiology/American Heart Association Pooled Cohort Equations model (B and D) in the full cohort (A, B)) and in the Mached cohort (C, D)
Disclosures:
Quazim Alayo indicated no relevant financial relationships.
Daniel Famutimi indicated no relevant financial relationships.
Malek Ayoub indicated no relevant financial relationships.
Parakkal Deepak: Abbvie – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Boehringer Ingelheim – Grant/Research Support. Fresenius Kabi – Consultant. Janssen – Grant/Research Support. Pfizer/Arena Pharmaceuticals – Grant/Research Support. Prometheus Biosciences – Grant/Research Support. Prometheus Labs – Grant/Research Support. Roche – Grant/Research Support, PI on a study. Sandoz – Advisory Committee/Board Member. Takeda – Grant/Research Support.
Quazim Alayo, MD, MSc, MMSc1, Daniel Famutimi, MBBS, MPH2, Malek Ayoub, MD1, Parakkal Deepak, MBBS, MS3. P3647 - Performance of ASCVD Risk Prediction Models in Individuals with Inflammatory Bowel Disease: A UK Biobank Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
