Tuesday Poster Session
Category: IBD
P3648 - A Functional Medicine Program for Patients With Inflammatory Bowel Disease and Improvement in Fecal Calprotectin Levels
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Thomas M. Strobel, MD
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Award: Presidential Poster Award
Thomas M. Strobel, MD1, Emily Spring, PA-C2, Sara Horst, MD, MPH1, Sarah Campbell, LCSW3, Randi Robbins, LCSW4, Robin Dalal, MD1, Elizabeth Scoville, MD, MSCI1, Baldeep Pabla, MD1, David Schwartz, MD5, Dawn Borromeo Beaulieu, MD1
1Vanderbilt University Medical Center, Nashville, TN; 2Vanderbilt IBD-FMC, Nashville, TN; 3Vanderbilt IBD Clinic, Nashville, TN; 4Vanderbilt Medical Center, Nashville, TN; 5Vanderbilt University Medical Center, Brentwood, TN
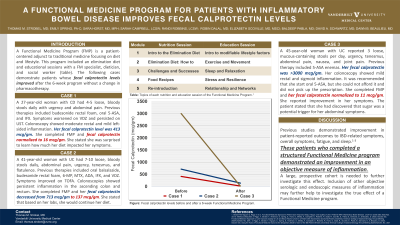
Introduction: Functional Medicine is a patient-centered adjunct to traditional medicine focusing on diet and lifestyle. This program includes an elimination diet and educational sessions with a Functional Medicine specialist, dietician, and social worker. The following cases demonstrate patients whose fecal calprotectin levels improved after the 6-week program.
Case Description/Methods: Case 1: A 27-year-old woman with Crohn’s Disease reported 4-5 loose, bloody stools daily, urgency, and abdominal pain. Previous therapies included budesonide rectal foam, oral mesalamine, and infliximab. Her symptoms worsened on vedolizumab and persisted on usetekinumab. Colonoscopy showed moderate rectal and mild left-sided inflammation. Fecal calprotectin level was 413 mcg/gm. She completed the Functional Medicine program and her fecal calprotectin level returned to normal. She reported that she was surprised how much her diet impacted her GI symptoms after paying more attention to what she ate.
Case 2: A 41-year-old woman with Ulcerative Colitis reported 7-10 loose, bloody stools per day, abdominal pain, urgency, tenesmus, and flatulence. Previous therapies included oral balsalazide, budesonide rectal foam, 6-mercaptopurine, methotrexate, adalimumab, infliximab, and vedolizumab. She achieved symptomatic improvement on tofacitinib, but serial colonoscopies showed persistent inflammation in the rectum and ascending colon. She completed the Functional Medicine program and her fecal calprotectin level decreased from 713 mcg/gm to 137 mcg/gm. She reported that although her symptoms were always minimal, based on her lab results, she would continue her elimination diet.
Case 3: A 45-year-old woman with Ulcerative Colitis reported 3 loose, mucous-containing stools per day, urgency, tenesmus, abdominal pain, nausea, and joint pain. Previous therapy included mesalamine enemas. Her fecal calprotectin was >3000 mcg/gm and colonoscopy showed mild rectal and sigmoid inflammation. She was prescribed oral mesalamine but could not afford it. She completed the Functional Medicine program and her fecal calprotectin level returned to normal. Her symptoms improved and she stated that she learned sugar was a potential trigger for her abdominal symptoms.
Discussion: Previous studies investigating Functional Medicine showed improvement in symptoms, fatigue, and sleep. These cases show improvement in fecal calprotectin. A larger, prospective design with other measures of inflammation is needed to further investigate this effect.
Disclosures:
Thomas M. Strobel, MD1, Emily Spring, PA-C2, Sara Horst, MD, MPH1, Sarah Campbell, LCSW3, Randi Robbins, LCSW4, Robin Dalal, MD1, Elizabeth Scoville, MD, MSCI1, Baldeep Pabla, MD1, David Schwartz, MD5, Dawn Borromeo Beaulieu, MD1. P3648 - A Functional Medicine Program for Patients With Inflammatory Bowel Disease and Improvement in Fecal Calprotectin Levels, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Thomas M. Strobel, MD1, Emily Spring, PA-C2, Sara Horst, MD, MPH1, Sarah Campbell, LCSW3, Randi Robbins, LCSW4, Robin Dalal, MD1, Elizabeth Scoville, MD, MSCI1, Baldeep Pabla, MD1, David Schwartz, MD5, Dawn Borromeo Beaulieu, MD1
1Vanderbilt University Medical Center, Nashville, TN; 2Vanderbilt IBD-FMC, Nashville, TN; 3Vanderbilt IBD Clinic, Nashville, TN; 4Vanderbilt Medical Center, Nashville, TN; 5Vanderbilt University Medical Center, Brentwood, TN
Introduction: Functional Medicine is a patient-centered adjunct to traditional medicine focusing on diet and lifestyle. This program includes an elimination diet and educational sessions with a Functional Medicine specialist, dietician, and social worker. The following cases demonstrate patients whose fecal calprotectin levels improved after the 6-week program.
Case Description/Methods: Case 1: A 27-year-old woman with Crohn’s Disease reported 4-5 loose, bloody stools daily, urgency, and abdominal pain. Previous therapies included budesonide rectal foam, oral mesalamine, and infliximab. Her symptoms worsened on vedolizumab and persisted on usetekinumab. Colonoscopy showed moderate rectal and mild left-sided inflammation. Fecal calprotectin level was 413 mcg/gm. She completed the Functional Medicine program and her fecal calprotectin level returned to normal. She reported that she was surprised how much her diet impacted her GI symptoms after paying more attention to what she ate.
Case 2: A 41-year-old woman with Ulcerative Colitis reported 7-10 loose, bloody stools per day, abdominal pain, urgency, tenesmus, and flatulence. Previous therapies included oral balsalazide, budesonide rectal foam, 6-mercaptopurine, methotrexate, adalimumab, infliximab, and vedolizumab. She achieved symptomatic improvement on tofacitinib, but serial colonoscopies showed persistent inflammation in the rectum and ascending colon. She completed the Functional Medicine program and her fecal calprotectin level decreased from 713 mcg/gm to 137 mcg/gm. She reported that although her symptoms were always minimal, based on her lab results, she would continue her elimination diet.
Case 3: A 45-year-old woman with Ulcerative Colitis reported 3 loose, mucous-containing stools per day, urgency, tenesmus, abdominal pain, nausea, and joint pain. Previous therapy included mesalamine enemas. Her fecal calprotectin was >3000 mcg/gm and colonoscopy showed mild rectal and sigmoid inflammation. She was prescribed oral mesalamine but could not afford it. She completed the Functional Medicine program and her fecal calprotectin level returned to normal. Her symptoms improved and she stated that she learned sugar was a potential trigger for her abdominal symptoms.
Discussion: Previous studies investigating Functional Medicine showed improvement in symptoms, fatigue, and sleep. These cases show improvement in fecal calprotectin. A larger, prospective design with other measures of inflammation is needed to further investigate this effect.
Disclosures:
Thomas Strobel indicated no relevant financial relationships.
Emily Spring indicated no relevant financial relationships.
Sara Horst: Abbvie – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. USB – Advisory Committee/Board Member, Consultant.
Sarah Campbell indicated no relevant financial relationships.
Randi Robbins indicated no relevant financial relationships.
Robin Dalal indicated no relevant financial relationships.
Elizabeth Scoville indicated no relevant financial relationships.
Baldeep Pabla indicated no relevant financial relationships.
David Schwartz: AbbVie – Advisory Committee/Board Member, Consultant. Genetech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant.
Dawn Borromeo Beaulieu: AbbVie – Advisory Committee/Board Member, Consultant. AndHealth – Consultant. Takeda – Advisory Committee/Board Member, Consultant.
Thomas M. Strobel, MD1, Emily Spring, PA-C2, Sara Horst, MD, MPH1, Sarah Campbell, LCSW3, Randi Robbins, LCSW4, Robin Dalal, MD1, Elizabeth Scoville, MD, MSCI1, Baldeep Pabla, MD1, David Schwartz, MD5, Dawn Borromeo Beaulieu, MD1. P3648 - A Functional Medicine Program for Patients With Inflammatory Bowel Disease and Improvement in Fecal Calprotectin Levels, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

