Tuesday Poster Session
Category: IBD
P3652 - Unveiling the Unforeseen: Parastomal Pyoderma Gangrenosum Eruption Following Secukinumab Initiation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AZ
Anas Zaher, MD
New York Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Anas Zaher, MD1, Michael Castillo, MD2
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2NYP Brooklyn Methodist, Brooklyn, NY
Introduction: Pyoderma Gangrenosum (PG) is a rare dermatologic inflammatory process characterized by painful and necrotic ulcerations mediated by neutrophil-predominant infiltrations in the dermal layer. PG has been associated with inflammatory bowel disease (IBD) in 41% and inflammatory arthritis in 20.5% of cases. We present a unique case of biologic-refractory ulcerative colitis (UC) requiring colectomy and end-ileostomy presenting with parastomal pyoderma gangrenosum (PPG) after initiation of Secukinumab.
Case Description/Methods: A 29-year-old male with biologic refractory UC and sacroiliitis presented to the hospital for symptoms of UC flare. His hospitalization was complicated by the development of fulminant colitis warranting an emergent total colectomy with end ileostomy. After a prolonged ICU course, the patient fully recovered and was discharged with follow up. Eight weeks after surgery, he noticed a painful ulcer surrounding his stoma site. On examination, his wound was erythematous, tender, pustular, with undermining borders consistent with PPG. It was noted that he was recently started on Secukinumab for worsening sacroiliitis by his rheumatologist. Secukinumab was discontinued and he was started on oral prednisone for PPG. Despite immunosuppression his lesion continued to progress and Anti-TNF therapy was considered however he had previously failed multiple medications and thus he was referred to the surgery for re-siting his ileostomy in anticipation of future J-pouch anastomosis. Surgical intervention in combination with oral and topical immunosuppression significantly improved the appearance and symptoms of his PPG.
Discussion: Secukinumab, a monoclonal antibody that selectively inhibits IL-17A, has primarily been used in the treatment of psoriasis and ankylosing spondylitis. Some studies have shown IL-17 inhibitors may be associated with exacerbations and new onset of IBD. The association between Secukinumab and the development of PG remains limited, with only a few published cases demonstrating a link. Ustekinumab has been utilized as a treatment option while others have resorted to surgical intervention. Further studies are necessary to develop a more comprehensive understanding of the role Secukinumab plays in the development of PG. This will help shed light on the potential mechanisms and establish clearer guidelines for the management of this condition. Caution should be exercised when considering Secukinumab in patients with PG, particularly in those with concomitant IBD.

Disclosures:
Anas Zaher, MD1, Michael Castillo, MD2. P3652 - Unveiling the Unforeseen: Parastomal Pyoderma Gangrenosum Eruption Following Secukinumab Initiation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2NYP Brooklyn Methodist, Brooklyn, NY
Introduction: Pyoderma Gangrenosum (PG) is a rare dermatologic inflammatory process characterized by painful and necrotic ulcerations mediated by neutrophil-predominant infiltrations in the dermal layer. PG has been associated with inflammatory bowel disease (IBD) in 41% and inflammatory arthritis in 20.5% of cases. We present a unique case of biologic-refractory ulcerative colitis (UC) requiring colectomy and end-ileostomy presenting with parastomal pyoderma gangrenosum (PPG) after initiation of Secukinumab.
Case Description/Methods: A 29-year-old male with biologic refractory UC and sacroiliitis presented to the hospital for symptoms of UC flare. His hospitalization was complicated by the development of fulminant colitis warranting an emergent total colectomy with end ileostomy. After a prolonged ICU course, the patient fully recovered and was discharged with follow up. Eight weeks after surgery, he noticed a painful ulcer surrounding his stoma site. On examination, his wound was erythematous, tender, pustular, with undermining borders consistent with PPG. It was noted that he was recently started on Secukinumab for worsening sacroiliitis by his rheumatologist. Secukinumab was discontinued and he was started on oral prednisone for PPG. Despite immunosuppression his lesion continued to progress and Anti-TNF therapy was considered however he had previously failed multiple medications and thus he was referred to the surgery for re-siting his ileostomy in anticipation of future J-pouch anastomosis. Surgical intervention in combination with oral and topical immunosuppression significantly improved the appearance and symptoms of his PPG.
Discussion: Secukinumab, a monoclonal antibody that selectively inhibits IL-17A, has primarily been used in the treatment of psoriasis and ankylosing spondylitis. Some studies have shown IL-17 inhibitors may be associated with exacerbations and new onset of IBD. The association between Secukinumab and the development of PG remains limited, with only a few published cases demonstrating a link. Ustekinumab has been utilized as a treatment option while others have resorted to surgical intervention. Further studies are necessary to develop a more comprehensive understanding of the role Secukinumab plays in the development of PG. This will help shed light on the potential mechanisms and establish clearer guidelines for the management of this condition. Caution should be exercised when considering Secukinumab in patients with PG, particularly in those with concomitant IBD.

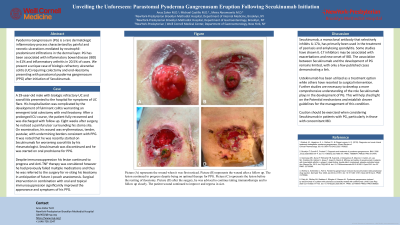
Figure: Picture (A) represents the wound when it was first noticed. Picture (B) represents the wound after a follow up. The lesion continued to progress despite being on optimal therapy for PPG. Picture (C) represents the lesion before the resiting of ileostomy. Picture (D) after the surgery, he was advised to continue taking immunotherapy and to follow up closely. The patient wound continued to improve and regress in size.
Disclosures:
Anas Zaher indicated no relevant financial relationships.
Michael Castillo indicated no relevant financial relationships.
Anas Zaher, MD1, Michael Castillo, MD2. P3652 - Unveiling the Unforeseen: Parastomal Pyoderma Gangrenosum Eruption Following Secukinumab Initiation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
