Tuesday Poster Session
Category: IBD
P3654 - A Case of Cutaneous Crohn’s Disease Without Intestinal Involvement
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Ariel A. Jordan, MD
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Ariel A. Jordan, MD, Fadi Hawa, MD, Mehwish Ahmed, MD, Matthew J. DiMagno, MD
University of Michigan, Ann Arbor, MI
Introduction: While extraintestinal manifestations are common in inflammatory bowel disease (IBD), especially Crohn’s disease (CD), cutaneous involvement is exceedingly rare. Cutaneous manifestations without intestinal involvement in CD have only been described in limited case reports. We present an unusual presentation of cutaneous genitourinary findings in a CD patient without intestinal involvement.
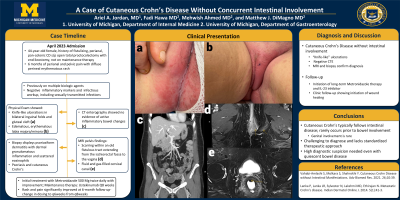
Case Description/Methods: A 44-year-old female with a history of fistulizing, perianal, pan-colonic CD s/p open total proctocolectomy with end ileostomy currently not on maintenance therapy was admitted for 6 months of abdominal, perianal, and pelvic pain associated with diffuse perineal erythematous rash. In terms of IBD history, she had been on multiple previous biologic agents, including Infliximab and Adalimumab on which she developed antibodies and Vedolizumab with Azathioprine on which she developed cerebellar meningioma complicated by seizures. Physical exam showed edematous and erythematous labia majora/minora extending down the bilateral anterior upper thighs with knife-like ulcerations in bilateral inguinal folds and gluteal cleft (a,b). Inflammatory markers, STI swabs, blood, and urine cultures were all negative. CT enterography showed no evidence of active inflammatory bowel changes (c). MRI pelvis demonstrated fluid and gas-filled cervical canal (d) and scarring within an old fistulous tract extending from ischiorectal fossa to the vagina (e). Biopsies showed psoriasiform dermatitis with dermal granulomatous inflammation and scattered eosinophils, consistent with psoriasis and cutaneous Crohn’s. The patient was discharged on Metronidazole 500 Mg twice daily with improving skin findings with plan to initiate Ustekinumab in the outpatient setting.
Discussion: Cutaneous Crohn’s disease typically follows intestinal disease and only rarely occurs prior to bowel involvement. Genital involvement in CD is rare, however, “knife-like” ulcerations are known to be pathognomonic for vulvar CD. Given its infrequency, the diagnosis of cutaneous Crohn’s is typically delayed and lacks a standardized therapeutic approach, though metronidazole and biologic therapy have shown efficacy in other cases, similar to our patient. Physicians should be aware of this rare presentation of CD especially in patients with unusual new skin findings but seemingly quiescent bowel disease.

Disclosures:
Ariel A. Jordan, MD, Fadi Hawa, MD, Mehwish Ahmed, MD, Matthew J. DiMagno, MD. P3654 - A Case of Cutaneous Crohn’s Disease Without Intestinal Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Michigan, Ann Arbor, MI
Introduction: While extraintestinal manifestations are common in inflammatory bowel disease (IBD), especially Crohn’s disease (CD), cutaneous involvement is exceedingly rare. Cutaneous manifestations without intestinal involvement in CD have only been described in limited case reports. We present an unusual presentation of cutaneous genitourinary findings in a CD patient without intestinal involvement.
Case Description/Methods: A 44-year-old female with a history of fistulizing, perianal, pan-colonic CD s/p open total proctocolectomy with end ileostomy currently not on maintenance therapy was admitted for 6 months of abdominal, perianal, and pelvic pain associated with diffuse perineal erythematous rash. In terms of IBD history, she had been on multiple previous biologic agents, including Infliximab and Adalimumab on which she developed antibodies and Vedolizumab with Azathioprine on which she developed cerebellar meningioma complicated by seizures. Physical exam showed edematous and erythematous labia majora/minora extending down the bilateral anterior upper thighs with knife-like ulcerations in bilateral inguinal folds and gluteal cleft (a,b). Inflammatory markers, STI swabs, blood, and urine cultures were all negative. CT enterography showed no evidence of active inflammatory bowel changes (c). MRI pelvis demonstrated fluid and gas-filled cervical canal (d) and scarring within an old fistulous tract extending from ischiorectal fossa to the vagina (e). Biopsies showed psoriasiform dermatitis with dermal granulomatous inflammation and scattered eosinophils, consistent with psoriasis and cutaneous Crohn’s. The patient was discharged on Metronidazole 500 Mg twice daily with improving skin findings with plan to initiate Ustekinumab in the outpatient setting.
Discussion: Cutaneous Crohn’s disease typically follows intestinal disease and only rarely occurs prior to bowel involvement. Genital involvement in CD is rare, however, “knife-like” ulcerations are known to be pathognomonic for vulvar CD. Given its infrequency, the diagnosis of cutaneous Crohn’s is typically delayed and lacks a standardized therapeutic approach, though metronidazole and biologic therapy have shown efficacy in other cases, similar to our patient. Physicians should be aware of this rare presentation of CD especially in patients with unusual new skin findings but seemingly quiescent bowel disease.

Figure: a) edematous and erythematous labia majora/minora b) knife-like ulcerations in bilateral inguinal folds c) lack of intestinal inflammation on CT enterography d) post-surgical soft tissue tract from vagina to left ischiorectal fossa (arrows) on MRI pelvis e) gas and fluid-filled cervix (arrow) on MRI pelvis
Disclosures:
Ariel Jordan indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Mehwish Ahmed indicated no relevant financial relationships.
Matthew DiMagno indicated no relevant financial relationships.
Ariel A. Jordan, MD, Fadi Hawa, MD, Mehwish Ahmed, MD, Matthew J. DiMagno, MD. P3654 - A Case of Cutaneous Crohn’s Disease Without Intestinal Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
