Tuesday Poster Session
Category: IBD
P3657 - A Case Report of Refractory UC With Associated SAPHO Treated With Tofacitinib
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Bryan J. Kim, MD
University of California, San Francisco
San Francisco, CA
Presenting Author(s)
Bryan J. Kim, MD, Kendall R. Beck, MD, Brett Dietz, MD
University of California, San Francisco, San Francisco, CA
Introduction: Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome is a rare inflammatory condition of the bone, joint, and skin associated with inflammatory bowel disease (IBD). Limited data exist on SAPHO management. We report a patient with ulcerative colitis (UC) with intractable headache diagnosed as SAPHO.
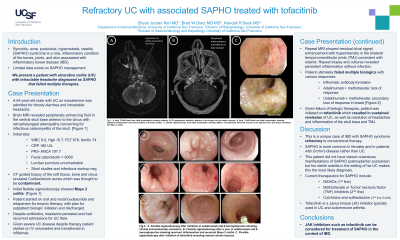
Case Description/Methods: A 54-year-old male with UC on mesalamine was admitted for bloody diarrhea and intractable headache. Brain MRI revealed peripherally enhancing fluid in the central skull base anterior to the clivus with retropharyngeal adenopathy concerning for infectious osteomyelitis. Labs revealed CRP 42.9, PR3-ANCA 197.7, fecal calprotectin > 8000. Lumbar puncture was unremarkable. CT-guided biopsy of the left nasopharynx, prevertebral soft tissue, and clivus revealed Cutibacterium acnes which was likely a contaminant, but the patient was given a 3-month course of ertapenem. Flexible sigmoidoscopy showed Mayo 2 colitis. This was treated with oral and rectal budesonide followed by infliximab due to persistent severe UC.
Despite antibiotic therapy, he had persistent headache and admissions for UC flare. Repeat MRI showed residual clival signal enhancement with hyperintensity in the bilateral temporomandibular joints (TMJ) consistent with osteitis. Repeat surgical biopsy and culture revealed chronic inflammatory changes. Whole body bone scan on biologic therapy showed no other involved sites. Immunodeficiency and genetic testing were negative. Patient did not achieve sustained remission of colitis or osteitis on infliximab with methotrexate (antibody formation) or ustekinumab with methotrexate (secondary loss of response of bowel and osteitis). Tofacitinib was initiated with sustained remission of UC and headache and resolved skull base and TMJ inflammation.
Discussion: This is a unique case of IBD with SAPHO syndrome refractory to conventional therapy. SAPHO is associated with IBD but more common in females and Crohn’s colitis. This patient did not have classic cutaneous manifestations of SAPHO but his isolated sterile osteitis in the context of IBD makes this the most likely diagnosis.
Treatment modalities for SAPHO include NSAIDs, methotrexate, bisphosphonates, and TNF inhibitors. Despite escalation of therapy, he had no sustained remission of UC or SAPHO. Janus kinase inhibitors are used in UC and autoimmune arthritis, therefore tofacitinib was tried with good success. This case demonstrates that tofacitinib is an option in the treatment of SAPHO in the context of IBD.
Disclosures:
Bryan J. Kim, MD, Kendall R. Beck, MD, Brett Dietz, MD. P3657 - A Case Report of Refractory UC With Associated SAPHO Treated With Tofacitinib, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of California, San Francisco, San Francisco, CA
Introduction: Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome is a rare inflammatory condition of the bone, joint, and skin associated with inflammatory bowel disease (IBD). Limited data exist on SAPHO management. We report a patient with ulcerative colitis (UC) with intractable headache diagnosed as SAPHO.
Case Description/Methods: A 54-year-old male with UC on mesalamine was admitted for bloody diarrhea and intractable headache. Brain MRI revealed peripherally enhancing fluid in the central skull base anterior to the clivus with retropharyngeal adenopathy concerning for infectious osteomyelitis. Labs revealed CRP 42.9, PR3-ANCA 197.7, fecal calprotectin > 8000. Lumbar puncture was unremarkable. CT-guided biopsy of the left nasopharynx, prevertebral soft tissue, and clivus revealed Cutibacterium acnes which was likely a contaminant, but the patient was given a 3-month course of ertapenem. Flexible sigmoidoscopy showed Mayo 2 colitis. This was treated with oral and rectal budesonide followed by infliximab due to persistent severe UC.
Despite antibiotic therapy, he had persistent headache and admissions for UC flare. Repeat MRI showed residual clival signal enhancement with hyperintensity in the bilateral temporomandibular joints (TMJ) consistent with osteitis. Repeat surgical biopsy and culture revealed chronic inflammatory changes. Whole body bone scan on biologic therapy showed no other involved sites. Immunodeficiency and genetic testing were negative. Patient did not achieve sustained remission of colitis or osteitis on infliximab with methotrexate (antibody formation) or ustekinumab with methotrexate (secondary loss of response of bowel and osteitis). Tofacitinib was initiated with sustained remission of UC and headache and resolved skull base and TMJ inflammation.
Discussion: This is a unique case of IBD with SAPHO syndrome refractory to conventional therapy. SAPHO is associated with IBD but more common in females and Crohn’s colitis. This patient did not have classic cutaneous manifestations of SAPHO but his isolated sterile osteitis in the context of IBD makes this the most likely diagnosis.
Treatment modalities for SAPHO include NSAIDs, methotrexate, bisphosphonates, and TNF inhibitors. Despite escalation of therapy, he had no sustained remission of UC or SAPHO. Janus kinase inhibitors are used in UC and autoimmune arthritis, therefore tofacitinib was tried with good success. This case demonstrates that tofacitinib is an option in the treatment of SAPHO in the context of IBD.
Disclosures:
Bryan Kim indicated no relevant financial relationships.
Kendall Beck indicated no relevant financial relationships.
Brett Dietz indicated no relevant financial relationships.
Bryan J. Kim, MD, Kendall R. Beck, MD, Brett Dietz, MD. P3657 - A Case Report of Refractory UC With Associated SAPHO Treated With Tofacitinib, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

