Tuesday Poster Session
Category: IBD
P3658 - Investigation and Management of a Curious Case of Campylobacter-Triggered Ulcerative Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Lubaba Haque, DO
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, NV
Presenting Author(s)
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Brianna Yee, MD3, Bhavana Bhaya, MD4
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2Kirk Kerkorian School of Medicine, Las Vegas, NV; 3University of Nevada, Las Vegas Kirk Kerkorian School of Medicine, Las Vegas, NV; 4North Las Vegas VA Medical Center, Las Vegas, NV
Introduction: Ulcerative colitis (UC), defined by inflammation and ulceration of the gastrointestinal tract, is one of two inflammatory bowel diseases (IBD). Symptoms of UC could be both erroneously attributed to and triggered by infections. We present a case of Campylobacter-triggered UC and discuss the importance of its proper management.
Case Description/Methods: A 51-year-old male with gastroesophageal reflux disease presents with abdominal cramping and watery diarrhea for 2 months, after returning from a trip to Mexico. He was admitted, found to be Campylobacter-positive, and was discharged with antibiotics, which he completed. However, he then had worsening symptoms with several bloody stools daily, diffuse abdominal pain, and fever, prompting readmission to the hospital.
On this second admission, the patient was tachycardic and febrile. Laboratory studies revealed leukocytosis of 22,900 K/mcL and normocytic anemia of 10.7 g/dL. C-reactive protein (CRP) and fecal calprotectin were elevated to 100.3 MG/L and 5,230 mcg/g, respectively. Imaging showed diffuse thickening of the colonic wall, particularly from the splenic flexure to the sigmoid colon. Findings were concerning for severe colitis, likely due to IBD.
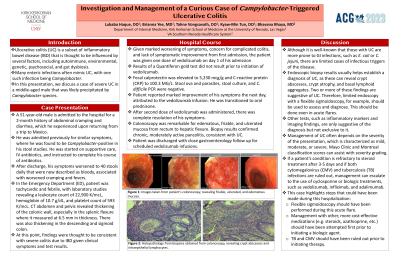
The patient was started on vedolizumab without confirmation of a negative tuberculosis (TB) test. His symptoms resolved. Repeat stool culture was negative. Colonoscopy revealed friable and ulcerated mucosa from rectum to hepatic flexure, with biopsy confirming ulcerative colitis. The patient was discharged with outpatient follow up.
Discussion: Despite what was thought to be initial proper management of his condition, the patient continued to complain of watery, and then bloody, diarrhea, with a fever and various laboratory abnormalities. This suggested an etiology other than simple Campylobacter infection. Although the patient improved, more coordinated management could have been provided. While it is crucial to entertain the possibility of IBD in this patient, starting immunosuppressive therapy without biopsy-confirmed IBD may have resulted in increased costs and harmful consequences. If the patient had latent TB, the immunosuppressive agent may have resulted in its reactivation. Performing a sigmoidoscopy initially may have helped guide therapy.
This case highlights the need for exploring different diagnoses in cases of persistent symptoms, and the importance of following proper guidelines and appropriate testing even if it does not result in harmful outcomes.

Disclosures:
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Brianna Yee, MD3, Bhavana Bhaya, MD4. P3658 - Investigation and Management of a Curious Case of Campylobacter-Triggered Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2Kirk Kerkorian School of Medicine, Las Vegas, NV; 3University of Nevada, Las Vegas Kirk Kerkorian School of Medicine, Las Vegas, NV; 4North Las Vegas VA Medical Center, Las Vegas, NV
Introduction: Ulcerative colitis (UC), defined by inflammation and ulceration of the gastrointestinal tract, is one of two inflammatory bowel diseases (IBD). Symptoms of UC could be both erroneously attributed to and triggered by infections. We present a case of Campylobacter-triggered UC and discuss the importance of its proper management.
Case Description/Methods: A 51-year-old male with gastroesophageal reflux disease presents with abdominal cramping and watery diarrhea for 2 months, after returning from a trip to Mexico. He was admitted, found to be Campylobacter-positive, and was discharged with antibiotics, which he completed. However, he then had worsening symptoms with several bloody stools daily, diffuse abdominal pain, and fever, prompting readmission to the hospital.
On this second admission, the patient was tachycardic and febrile. Laboratory studies revealed leukocytosis of 22,900 K/mcL and normocytic anemia of 10.7 g/dL. C-reactive protein (CRP) and fecal calprotectin were elevated to 100.3 MG/L and 5,230 mcg/g, respectively. Imaging showed diffuse thickening of the colonic wall, particularly from the splenic flexure to the sigmoid colon. Findings were concerning for severe colitis, likely due to IBD.
The patient was started on vedolizumab without confirmation of a negative tuberculosis (TB) test. His symptoms resolved. Repeat stool culture was negative. Colonoscopy revealed friable and ulcerated mucosa from rectum to hepatic flexure, with biopsy confirming ulcerative colitis. The patient was discharged with outpatient follow up.
Discussion: Despite what was thought to be initial proper management of his condition, the patient continued to complain of watery, and then bloody, diarrhea, with a fever and various laboratory abnormalities. This suggested an etiology other than simple Campylobacter infection. Although the patient improved, more coordinated management could have been provided. While it is crucial to entertain the possibility of IBD in this patient, starting immunosuppressive therapy without biopsy-confirmed IBD may have resulted in increased costs and harmful consequences. If the patient had latent TB, the immunosuppressive agent may have resulted in its reactivation. Performing a sigmoidoscopy initially may have helped guide therapy.
This case highlights the need for exploring different diagnoses in cases of persistent symptoms, and the importance of following proper guidelines and appropriate testing even if it does not result in harmful outcomes.

Figure: Images from colonoscopy performed during the second admission. Ulcerated and friable mucosa visible throughout the colon, indicative of ulcerative colitis.
Disclosures:
Lubaba Haque indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Tahne Vongsavath indicated no relevant financial relationships.
Brianna Yee indicated no relevant financial relationships.
Bhavana Bhaya indicated no relevant financial relationships.
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Brianna Yee, MD3, Bhavana Bhaya, MD4. P3658 - Investigation and Management of a Curious Case of Campylobacter-Triggered Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
