Tuesday Poster Session
Category: IBD
P3662 - An Unusual Case of Colitis Following HIPEC Therapy: Cause or Coincidence?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kavea Panneerselvam, MD
University of Texas Health Science Center at San Antonio
San Antonio, TX
Presenting Author(s)
Kavea Panneerselvam, MD1, Priyadarshini Loganathan, MD2, Mahesh Gajendran, MD, MPH1, Laura Rosenkranz, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy (HIPEC) is a treatment used in patients with peritoneal metastases from various cancers. HIPEC has several well-described gastrointestinal side effects, including bowel obstruction, ileus, bowel leaks, and fistulas. Here, we present an interesting case of ulcerative colitis (UC) as a delayed complication of HIPEC.
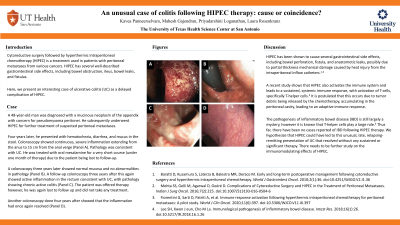
Case Description/Methods: A 48-year-old man was diagnosed with a mucinous neoplasm of the appendix with concern for pseudomyxoma peritonei. He subsequently underwent HIPEC for further treatment of suspected peritoneal metastases. Four years later, he presented with hematochezia, diarrhea, and mucus in the stool. Colonoscopy showed continuous, severe inflammation extending from the anus to 15 cm from the anal verge (Panel A). Pathology was consistent with UC. He was treated with oral mesalamine for a very short course (under one month of therapy) due to the patient being lost to follow-up. A colonoscopy three years later showed normal mucosa and no abnormalities in pathology (Panel B). A follow-up colonoscopy three years after this again showed active inflammation in the rectum consistent with UC, with pathology showing chronic active colitis (Panel C). The patient was offered therapy however, he was again lost to follow up and did not take any treatment. Another colonoscopy done four years after showed that the inflammation had once again resolved (Panel D).
Discussion: HIPEC has been shown to cause several gastrointestinal side effects, including bowel perforation, fistula, and anastomotic leaks, possibly due to partial thickness mechanical damage caused by heat injury from the intraperitoneal inflow catheters. A recent study shows that HIPEC also activates the immune system and leads to a sustained, systemic immune response, with activation of T-cells, specifically T-helper cells. It is postulated that this occurs due to tumor debris being released by the chemotherapy, accumulating in the peritoneal cavity, leading to an adaptive immune response. The pathogenesis of inflammatory bowel disease (IBD) is still largely a mystery, however it is known that T-helper cells play a large role. Thus far, there have been no cases reported of IBD following HIPEC therapy. We hypothesize that HIPEC could have led to this unusual, late, relapsing-remitting presentation of UC that resolved without any sustained or significant therapy. There needs to be further study on the immunomodulating effects of HIPEC.

Disclosures:
Kavea Panneerselvam, MD1, Priyadarshini Loganathan, MD2, Mahesh Gajendran, MD, MPH1, Laura Rosenkranz, MD1. P3662 - An Unusual Case of Colitis Following HIPEC Therapy: Cause or Coincidence?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy (HIPEC) is a treatment used in patients with peritoneal metastases from various cancers. HIPEC has several well-described gastrointestinal side effects, including bowel obstruction, ileus, bowel leaks, and fistulas. Here, we present an interesting case of ulcerative colitis (UC) as a delayed complication of HIPEC.
Case Description/Methods: A 48-year-old man was diagnosed with a mucinous neoplasm of the appendix with concern for pseudomyxoma peritonei. He subsequently underwent HIPEC for further treatment of suspected peritoneal metastases. Four years later, he presented with hematochezia, diarrhea, and mucus in the stool. Colonoscopy showed continuous, severe inflammation extending from the anus to 15 cm from the anal verge (Panel A). Pathology was consistent with UC. He was treated with oral mesalamine for a very short course (under one month of therapy) due to the patient being lost to follow-up. A colonoscopy three years later showed normal mucosa and no abnormalities in pathology (Panel B). A follow-up colonoscopy three years after this again showed active inflammation in the rectum consistent with UC, with pathology showing chronic active colitis (Panel C). The patient was offered therapy however, he was again lost to follow up and did not take any treatment. Another colonoscopy done four years after showed that the inflammation had once again resolved (Panel D).
Discussion: HIPEC has been shown to cause several gastrointestinal side effects, including bowel perforation, fistula, and anastomotic leaks, possibly due to partial thickness mechanical damage caused by heat injury from the intraperitoneal inflow catheters. A recent study shows that HIPEC also activates the immune system and leads to a sustained, systemic immune response, with activation of T-cells, specifically T-helper cells. It is postulated that this occurs due to tumor debris being released by the chemotherapy, accumulating in the peritoneal cavity, leading to an adaptive immune response. The pathogenesis of inflammatory bowel disease (IBD) is still largely a mystery, however it is known that T-helper cells play a large role. Thus far, there have been no cases reported of IBD following HIPEC therapy. We hypothesize that HIPEC could have led to this unusual, late, relapsing-remitting presentation of UC that resolved without any sustained or significant therapy. There needs to be further study on the immunomodulating effects of HIPEC.

Figure: Panel A: First colonoscopy done 4 years after HIPEC that showed severe rectal inflammation. Panel B: Second colonoscopy with normal rectal mucosa. Panel C: Third colonoscopy with severe inflammation in the rectum. Panel D: Fourth colonoscopy with normal rectal mucosa,
Disclosures:
Kavea Panneerselvam indicated no relevant financial relationships.
Priyadarshini Loganathan indicated no relevant financial relationships.
Mahesh Gajendran indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Kavea Panneerselvam, MD1, Priyadarshini Loganathan, MD2, Mahesh Gajendran, MD, MPH1, Laura Rosenkranz, MD1. P3662 - An Unusual Case of Colitis Following HIPEC Therapy: Cause or Coincidence?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
