Tuesday Poster Session
Category: IBD
P3669 - Successful Multidisciplinary Treatment of the Rare Pathology of Vulvar Crohn’s Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Michael Ladna, MD
University of Florida
Gainesville, FL
Presenting Author(s)
Michael Ladna, MD, Kelcie Brown, MD, Raed Ghaleb Eid Al Yacoub, MD
University of Florida, Gainesville, FL
Introduction: Vulvar Crohn’s disease is a rare manifestation of Crohn’s disease that can present a diagnostic dilemma and be mistaken for other pathologies such as pyoderma gangrenosum, sarcoidosis, herpes simplex, or Bechet’s. Up to 30% of patients with vulvar Crohn’s lack gastrointestinal manifestations of Crohn’s disease at the time of diagnosis further increasing difficulty of attaining an accurate diagnosis.
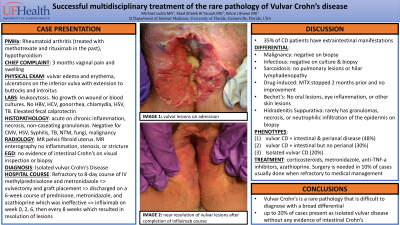
Case Description/Methods: A woman in her 50’s with a past medical history of rheumatoid arthritis and hypothyroidism presented with 3 months of progressively worsening vaginal pain and swelling. Physical exam revealed vulvar edema and erythema, ulcerations of the inferior vulva that extended to the buttocks and introitus with erythema and superficial erosions. Biopsies of the vagina showed extensive acute and chronic inflammation, necrosis, and granulomas without concern for malignancy which was consistent with a diagnosis of cutaneous Crohn’s disease. MR enterography, upper endoscopy, and lower endoscopy revealed no gastrointestinal manifestations of Crohn’s disease. She was treated with IV methylprednisolone 60mg daily for 8 days and PO metronidazole. She had a vulvectomy and graft placement during her initial hospital visit. She was discharged on prednisone, metronidazole, and azathioprine. Due to inadequate response after 6 weeks of treatment, she was started on infliximab and completed three infusions at weeks 0, 2, 6 with subsequent resolution of all cutaneous lesions.
Discussion: Genital manifestations of Crohn's are seen mostly in female patients. Vulvar Crohn’s is a rare metastatic manifestation of CD. Vulvar Crohn’s presents a diagnostic challenge with median time to diagnosis of 3.5 years and patients often seeing multiple specialists prior to establishment of correct diagnosis. Vulvar findings include edema, labial hypertrophy, lymphangiectasia, knife-like fissures, ulcerations, abscesses, and fistulas while histology shows noncaseating granulomas. Up to 30% of cases occurred in the absence of gastrointestinal disease activity. The most common first-line therapy is systemic corticosteroids and metronidazole. If the initial medical therapy should fail then escalation to biologics such as anti-TNF-a inhibitors should be trialed. Surgery is reserved for cases that do not respond to medical therapy. Available surgical approaches may include incision and drainage of abscesses, local resection of the lesion, vulvectomy, excision of pedunculated tags, and/or laser treatment of lymphangiectasias.

Disclosures:
Michael Ladna, MD, Kelcie Brown, MD, Raed Ghaleb Eid Al Yacoub, MD. P3669 - Successful Multidisciplinary Treatment of the Rare Pathology of Vulvar Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Florida, Gainesville, FL
Introduction: Vulvar Crohn’s disease is a rare manifestation of Crohn’s disease that can present a diagnostic dilemma and be mistaken for other pathologies such as pyoderma gangrenosum, sarcoidosis, herpes simplex, or Bechet’s. Up to 30% of patients with vulvar Crohn’s lack gastrointestinal manifestations of Crohn’s disease at the time of diagnosis further increasing difficulty of attaining an accurate diagnosis.
Case Description/Methods: A woman in her 50’s with a past medical history of rheumatoid arthritis and hypothyroidism presented with 3 months of progressively worsening vaginal pain and swelling. Physical exam revealed vulvar edema and erythema, ulcerations of the inferior vulva that extended to the buttocks and introitus with erythema and superficial erosions. Biopsies of the vagina showed extensive acute and chronic inflammation, necrosis, and granulomas without concern for malignancy which was consistent with a diagnosis of cutaneous Crohn’s disease. MR enterography, upper endoscopy, and lower endoscopy revealed no gastrointestinal manifestations of Crohn’s disease. She was treated with IV methylprednisolone 60mg daily for 8 days and PO metronidazole. She had a vulvectomy and graft placement during her initial hospital visit. She was discharged on prednisone, metronidazole, and azathioprine. Due to inadequate response after 6 weeks of treatment, she was started on infliximab and completed three infusions at weeks 0, 2, 6 with subsequent resolution of all cutaneous lesions.
Discussion: Genital manifestations of Crohn's are seen mostly in female patients. Vulvar Crohn’s is a rare metastatic manifestation of CD. Vulvar Crohn’s presents a diagnostic challenge with median time to diagnosis of 3.5 years and patients often seeing multiple specialists prior to establishment of correct diagnosis. Vulvar findings include edema, labial hypertrophy, lymphangiectasia, knife-like fissures, ulcerations, abscesses, and fistulas while histology shows noncaseating granulomas. Up to 30% of cases occurred in the absence of gastrointestinal disease activity. The most common first-line therapy is systemic corticosteroids and metronidazole. If the initial medical therapy should fail then escalation to biologics such as anti-TNF-a inhibitors should be trialed. Surgery is reserved for cases that do not respond to medical therapy. Available surgical approaches may include incision and drainage of abscesses, local resection of the lesion, vulvectomy, excision of pedunculated tags, and/or laser treatment of lymphangiectasias.

Figure: Photograph of the vagina at the time of diagnosis showing vulvar edema and erythema, ulcerations of the inferior vulva that extended to the buttocks and introitus with erythema and superficial erosions
Disclosures:
Michael Ladna indicated no relevant financial relationships.
Kelcie Brown indicated no relevant financial relationships.
Raed Ghaleb Eid Al Yacoub indicated no relevant financial relationships.
Michael Ladna, MD, Kelcie Brown, MD, Raed Ghaleb Eid Al Yacoub, MD. P3669 - Successful Multidisciplinary Treatment of the Rare Pathology of Vulvar Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
