Tuesday Poster Session
Category: IBD
P3671 - Ischemic Proctitis Masquerading as Crohn’s Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Tyrell Daniel, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Cierra Smith, DO1, Tyrell Daniel, MD1, Heitham Abdul-Baki, MD1, Michael Landau, MD2, Ethan Powell, DO1, Stacey B. Miller, MD3
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3AHN Wexford Hospital, Wexford, PA
Introduction: The colon is the most common part of the gastrointestinal tract to develop ischemia. Rectal involvement is uncommon & isolated rectal ischemia even more so due to rich vascular supply. Here we present a case of isolated ischemic proctitis in a patient with suspected inflammatory bowel disease (IBD).
Case Description/Methods: A mid 30s patient with history of postural orthostatic tachycardia syndrome & migraines was initially seen for a 2 month history of 6-7 loose stools a day. This was associated with cramping, intermittent bleeding & was temporally related to development of erythema nodosum. Initial work up, including infectious, thyroid & celiac studies, upper, lower & capsule endoscopy, was unremarkable. Notably Sacchromyces cerviciae IgG was elevated to 31.
They presented 3 months later with hematochezia. Endoscopy noted diffuse ulceration throughout the rectum with two visible vessels treated with epinephrine & clips. Biopsies showed non-specific inflammation & stool was Clostridium difficile positive for which they completed 14 days of oral vancomycin. After 1 month, diarrhea improved with evidence of endoscopic & microscopic healing with the treatment of C. difficile alone.
Six months later, they represented with hematochezia. Infectious disease workup was unrevealing & endoscopy showed multiple rectal ulcers & active colitis. Endoscopic findings were consistent with Crohn’s disease and they were started on usetekinumab. Due to clinical progression, therapy was transitioned to infliximab 2 months later with initial clinical & endoscopic improvement.
A year after starting infliximab they presented with recurrent rectal bleeding & severe abdominal pain. Endoscopy revealed ischemic proctitis & necrosis requiring laparoscopic proctectomy with end colostomy. Pathology was consistent with ischemia without evidence of IBD. Multidisciplinary review with gastroenterology, colorectal surgery, radiology & pathology revealed no clear etiology of ischemia. No evidence of trauma, volvulus, prolapse, mesenteric compromise, vascular anomalies or vasculitis was identified & review of prior endoscopic results still seemed most consistent with Crohn’s disease.
Discussion: Ischemic proctitis is a rare clinical entity, often the result of a low flow state, thromboembolism, severe atherosclerotic disease or aortic interventions. Our patient’s case presented diagnostic challenges based on the chronicity of their course, no overt risk factors for rectal ischemia & overall clinical picture consistent with IBD.

Disclosures:
Cierra Smith, DO1, Tyrell Daniel, MD1, Heitham Abdul-Baki, MD1, Michael Landau, MD2, Ethan Powell, DO1, Stacey B. Miller, MD3. P3671 - Ischemic Proctitis Masquerading as Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3AHN Wexford Hospital, Wexford, PA
Introduction: The colon is the most common part of the gastrointestinal tract to develop ischemia. Rectal involvement is uncommon & isolated rectal ischemia even more so due to rich vascular supply. Here we present a case of isolated ischemic proctitis in a patient with suspected inflammatory bowel disease (IBD).
Case Description/Methods: A mid 30s patient with history of postural orthostatic tachycardia syndrome & migraines was initially seen for a 2 month history of 6-7 loose stools a day. This was associated with cramping, intermittent bleeding & was temporally related to development of erythema nodosum. Initial work up, including infectious, thyroid & celiac studies, upper, lower & capsule endoscopy, was unremarkable. Notably Sacchromyces cerviciae IgG was elevated to 31.
They presented 3 months later with hematochezia. Endoscopy noted diffuse ulceration throughout the rectum with two visible vessels treated with epinephrine & clips. Biopsies showed non-specific inflammation & stool was Clostridium difficile positive for which they completed 14 days of oral vancomycin. After 1 month, diarrhea improved with evidence of endoscopic & microscopic healing with the treatment of C. difficile alone.
Six months later, they represented with hematochezia. Infectious disease workup was unrevealing & endoscopy showed multiple rectal ulcers & active colitis. Endoscopic findings were consistent with Crohn’s disease and they were started on usetekinumab. Due to clinical progression, therapy was transitioned to infliximab 2 months later with initial clinical & endoscopic improvement.
A year after starting infliximab they presented with recurrent rectal bleeding & severe abdominal pain. Endoscopy revealed ischemic proctitis & necrosis requiring laparoscopic proctectomy with end colostomy. Pathology was consistent with ischemia without evidence of IBD. Multidisciplinary review with gastroenterology, colorectal surgery, radiology & pathology revealed no clear etiology of ischemia. No evidence of trauma, volvulus, prolapse, mesenteric compromise, vascular anomalies or vasculitis was identified & review of prior endoscopic results still seemed most consistent with Crohn’s disease.
Discussion: Ischemic proctitis is a rare clinical entity, often the result of a low flow state, thromboembolism, severe atherosclerotic disease or aortic interventions. Our patient’s case presented diagnostic challenges based on the chronicity of their course, no overt risk factors for rectal ischemia & overall clinical picture consistent with IBD.

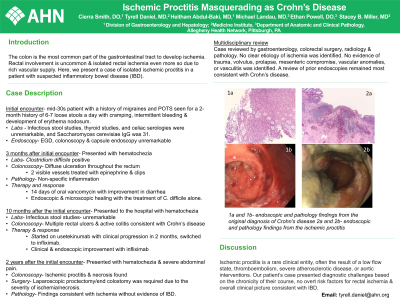
Figure: 1a and 1b are the representative endoscopic and pathology findings from the original diagnosis of Crohn's disease
2a and 2b are the representative endoscopic and pathology findings from the ischemic proctitis
2a and 2b are the representative endoscopic and pathology findings from the ischemic proctitis
Disclosures:
Cierra Smith indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Heitham Abdul-Baki indicated no relevant financial relationships.
Michael Landau indicated no relevant financial relationships.
Ethan Powell indicated no relevant financial relationships.
Stacey Miller indicated no relevant financial relationships.
Cierra Smith, DO1, Tyrell Daniel, MD1, Heitham Abdul-Baki, MD1, Michael Landau, MD2, Ethan Powell, DO1, Stacey B. Miller, MD3. P3671 - Ischemic Proctitis Masquerading as Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
