Tuesday Poster Session
Category: IBD
P3672 - Neutropenic Enterocolitis in a Patient With a History of Crohn’s Disease and Ileocecal Resection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Dariush Shahsavari, MD
Medical College of Georgia
Augusta, GA
Presenting Author(s)
Dariush Shahsavari, MD1, Praneeth Kudaravalli, MD2, Kwabena Adu-Gyamfi, MD3, Evangelos Tsipotis, MD2
1Medical College of Georgia, Augusta, GA; 2Augusta University, Augusta, GA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Neutropenic enterocolitis (Typhlitis) is a life threatening, necrotizing condition that primarily affects neutropenic patients. Pathogenesis involves factors such as mucosal injury from drugs or toxins, neutropenia and impaired host defense to invasion by bacteria. The diagnosis of neutropenic enterocolitis in patients with Crohn’s Disease (CD) can be challenging. We present a challenging case of severe neutropenic enterocolitis in a patient with Crohn’s Disease.
Case Description/Methods: Our patient is a 30-year-old female with a history of ileal CD diagnosed 5 years prior to presentation. She did not achieve deep remission on Adalimumab, Infliximab, Vedolizumab and Ustekinumab. Ultimately, she underwent ileocecal resection two years after diagnosis and started on Certolizumab Pegol post operatively with sustained deep remission. She was recently diagnosed with acute myeloblastic leukemia (AML) and underwent Daunorubicin induction therapy, followed by Cytarabine consolidation therapy for two cycles, followed by an allogenic stem cell transplant. Four days after the transplant, the patient developed new-onset right abdominal pain and watery diarrhea. Examination revealed significant tenderness in the RLQ, abdominal distention, tachycardia, and a fever of 39.5 oC. Labs showed undetectable white blood cell count, a hemoglobin of 7.6 gr/dL, platelet count of 17,000/mm3, and C-reactive protein of 22.2 mg/dL. Sputum, blood and urine cultures were negative as well as stool multi-pathogen and Clostridium difficile tests. Abdominal CT scan revealed long-segment thickening of the neo-terminal ileum with trilaminar enhancement, reactive mesenteric lymphadenopathy without signs of perforation. She started on broad spectrum antimicrobials with no significant response. Upon further investigation, it was discovered that she had a colonoscopy one month prior to presentation at another facility which showed no evidence of active CD. Neutropenic enterocolitis was suspected. Filgrastim was added to her antimicrobial regimen. Gradually, the patient's symptoms improved as her pancytopenia resolved, and she was eventually discharged home.
Discussion: Neutropenic enterocolitis can often mimic active IBD flare. Even though neutropenia makes active CD less likely it still should be in the differential. Colonoscopy might not be possible due to risk of complications in the setting of suspected neutropenic enterocolitis. Detailed history, examination, laboratory and imaging findings are important to make the diagnosis.

Disclosures:
Dariush Shahsavari, MD1, Praneeth Kudaravalli, MD2, Kwabena Adu-Gyamfi, MD3, Evangelos Tsipotis, MD2. P3672 - Neutropenic Enterocolitis in a Patient With a History of Crohn’s Disease and Ileocecal Resection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Medical College of Georgia, Augusta, GA; 2Augusta University, Augusta, GA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Neutropenic enterocolitis (Typhlitis) is a life threatening, necrotizing condition that primarily affects neutropenic patients. Pathogenesis involves factors such as mucosal injury from drugs or toxins, neutropenia and impaired host defense to invasion by bacteria. The diagnosis of neutropenic enterocolitis in patients with Crohn’s Disease (CD) can be challenging. We present a challenging case of severe neutropenic enterocolitis in a patient with Crohn’s Disease.
Case Description/Methods: Our patient is a 30-year-old female with a history of ileal CD diagnosed 5 years prior to presentation. She did not achieve deep remission on Adalimumab, Infliximab, Vedolizumab and Ustekinumab. Ultimately, she underwent ileocecal resection two years after diagnosis and started on Certolizumab Pegol post operatively with sustained deep remission. She was recently diagnosed with acute myeloblastic leukemia (AML) and underwent Daunorubicin induction therapy, followed by Cytarabine consolidation therapy for two cycles, followed by an allogenic stem cell transplant. Four days after the transplant, the patient developed new-onset right abdominal pain and watery diarrhea. Examination revealed significant tenderness in the RLQ, abdominal distention, tachycardia, and a fever of 39.5 oC. Labs showed undetectable white blood cell count, a hemoglobin of 7.6 gr/dL, platelet count of 17,000/mm3, and C-reactive protein of 22.2 mg/dL. Sputum, blood and urine cultures were negative as well as stool multi-pathogen and Clostridium difficile tests. Abdominal CT scan revealed long-segment thickening of the neo-terminal ileum with trilaminar enhancement, reactive mesenteric lymphadenopathy without signs of perforation. She started on broad spectrum antimicrobials with no significant response. Upon further investigation, it was discovered that she had a colonoscopy one month prior to presentation at another facility which showed no evidence of active CD. Neutropenic enterocolitis was suspected. Filgrastim was added to her antimicrobial regimen. Gradually, the patient's symptoms improved as her pancytopenia resolved, and she was eventually discharged home.
Discussion: Neutropenic enterocolitis can often mimic active IBD flare. Even though neutropenia makes active CD less likely it still should be in the differential. Colonoscopy might not be possible due to risk of complications in the setting of suspected neutropenic enterocolitis. Detailed history, examination, laboratory and imaging findings are important to make the diagnosis.

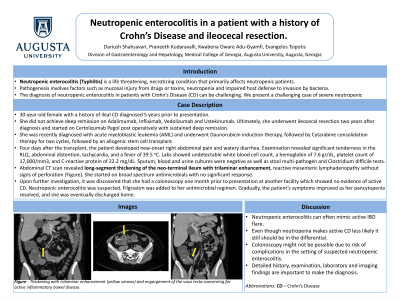
Figure: Figure 1- Thickening with trilaminar enhancement (yellow arrows) and engorgement of the vasa recta concerning for active inflammatory bowel disease.
Disclosures:
Dariush Shahsavari indicated no relevant financial relationships.
Praneeth Kudaravalli indicated no relevant financial relationships.
Kwabena Adu-Gyamfi indicated no relevant financial relationships.
Evangelos Tsipotis indicated no relevant financial relationships.
Dariush Shahsavari, MD1, Praneeth Kudaravalli, MD2, Kwabena Adu-Gyamfi, MD3, Evangelos Tsipotis, MD2. P3672 - Neutropenic Enterocolitis in a Patient With a History of Crohn’s Disease and Ileocecal Resection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
