Tuesday Poster Session
Category: IBD
P3677 - An Unusual Pulmonary Presentation of Inflammatory Bowel Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kyle M. Pierce, DO
University of Arizona-Phoenix
Phoenix, AZ
Presenting Author(s)
Award: Presidential Poster Award
Kyle M. Pierce, DO1, Anna L.. Silverman, MD2, Sailaja Pisipati, MBBS3, Lucinda A. Harris, MD2, Kevin Ruff, MD2, Cyril Varghese, MD2, Suryakanth Gurudu, MD2
1University of Arizona-Phoenix, Phoenix, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Extraintestinal manifestations (EIMs) in inflammatory bowel disease (IBD) may develop at any time along the course of the disease and can affect almost any organ system. While less common, some patients will have significant EIMs prior to the formal diagnosis of IBD. EIMs occur in nearly half of patients with IBD. Additionally, pulmonary EIMs in IBD have been recognized in all anatomical sites of the pulmonary tree including inflammation of the upper airway, bronchi, bronchioles, and lung parenchyma. We highlight this case both to raise awareness surrounding pulmonary EIMs as well as significant EIMs present prior to diagnosis of IBD.
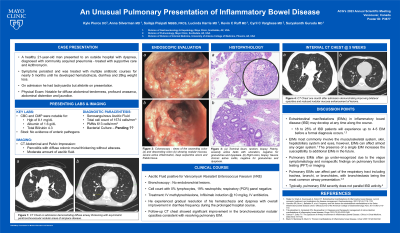
Case Description/Methods: A previously healthy 21-year-old man presented initially with significant dyspnea and infiltrates on chest x-ray. He was presumed to have community acquired pneumonia and treated with azithromycin. Subsequently, he was hospitalized due to continued dyspnea and treated with expanded spectrum antibiotics for what was thought to be worsening pneumonia. It was not until five months after the onset of significant dyspnea that he began experiencing hematochezia and a 28 kg weight loss.
On initial presentation, he was tachycardic but afebrile. His physical exam demonstrated anasarca with diffuse abdominal tenderness and fluid wave. Chest CT revealed asymmetric bronchovesicular nodular areas of airspace disease with diffuse airway thickening and scattered ground glass opacification. Colonoscopy demonstrated friable nodular mucosa with deep serpiginous ulcerations in the entire colon in addition to significant segmental ulcerations in the terminal ileum. He was treated with IV methylprednisolone, Infliximab, and IV antibiotics. He experienced gradual resolution of his dyspnea and hematochezia with overall improvement in diarrhea frequency during the hospital course. A follow up CT chest showed significant improvement in the bronchovesicular opacities consistent with resolving pulmonary EIM.
Discussion: This case is unique by the fact that our patient initially presented with a chief complaint of dyspnea as his initial manifestation of an EIM prior to the onset of luminal GI symptoms and diagnosis IBD. This presentation was a diagnostic challenge until his Crohn’s Disease symptoms manifested. This case underscores the importance of keeping a broad differential, candid communication, and collaboration between a large multidisciplinary team to efficiently arrive at the correct diagnosis and treatment.
Disclosures:
Kyle M. Pierce, DO1, Anna L.. Silverman, MD2, Sailaja Pisipati, MBBS3, Lucinda A. Harris, MD2, Kevin Ruff, MD2, Cyril Varghese, MD2, Suryakanth Gurudu, MD2. P3677 - An Unusual Pulmonary Presentation of Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Kyle M. Pierce, DO1, Anna L.. Silverman, MD2, Sailaja Pisipati, MBBS3, Lucinda A. Harris, MD2, Kevin Ruff, MD2, Cyril Varghese, MD2, Suryakanth Gurudu, MD2
1University of Arizona-Phoenix, Phoenix, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Extraintestinal manifestations (EIMs) in inflammatory bowel disease (IBD) may develop at any time along the course of the disease and can affect almost any organ system. While less common, some patients will have significant EIMs prior to the formal diagnosis of IBD. EIMs occur in nearly half of patients with IBD. Additionally, pulmonary EIMs in IBD have been recognized in all anatomical sites of the pulmonary tree including inflammation of the upper airway, bronchi, bronchioles, and lung parenchyma. We highlight this case both to raise awareness surrounding pulmonary EIMs as well as significant EIMs present prior to diagnosis of IBD.
Case Description/Methods: A previously healthy 21-year-old man presented initially with significant dyspnea and infiltrates on chest x-ray. He was presumed to have community acquired pneumonia and treated with azithromycin. Subsequently, he was hospitalized due to continued dyspnea and treated with expanded spectrum antibiotics for what was thought to be worsening pneumonia. It was not until five months after the onset of significant dyspnea that he began experiencing hematochezia and a 28 kg weight loss.
On initial presentation, he was tachycardic but afebrile. His physical exam demonstrated anasarca with diffuse abdominal tenderness and fluid wave. Chest CT revealed asymmetric bronchovesicular nodular areas of airspace disease with diffuse airway thickening and scattered ground glass opacification. Colonoscopy demonstrated friable nodular mucosa with deep serpiginous ulcerations in the entire colon in addition to significant segmental ulcerations in the terminal ileum. He was treated with IV methylprednisolone, Infliximab, and IV antibiotics. He experienced gradual resolution of his dyspnea and hematochezia with overall improvement in diarrhea frequency during the hospital course. A follow up CT chest showed significant improvement in the bronchovesicular opacities consistent with resolving pulmonary EIM.
Discussion: This case is unique by the fact that our patient initially presented with a chief complaint of dyspnea as his initial manifestation of an EIM prior to the onset of luminal GI symptoms and diagnosis IBD. This presentation was a diagnostic challenge until his Crohn’s Disease symptoms manifested. This case underscores the importance of keeping a broad differential, candid communication, and collaboration between a large multidisciplinary team to efficiently arrive at the correct diagnosis and treatment.
Disclosures:
Kyle Pierce indicated no relevant financial relationships.
Anna Silverman indicated no relevant financial relationships.
Sailaja Pisipati indicated no relevant financial relationships.
Lucinda Harris: AbbVie – Consultant. Ardelyx – Consultant. Gemelli Biotech – Advisor or Review Panel Member. Mahana – Consultant. QOL – Consultant. Salix – Consultant. takeda – Grant/Research Support.
Kevin Ruff indicated no relevant financial relationships.
Cyril Varghese indicated no relevant financial relationships.
Suryakanth Gurudu indicated no relevant financial relationships.
Kyle M. Pierce, DO1, Anna L.. Silverman, MD2, Sailaja Pisipati, MBBS3, Lucinda A. Harris, MD2, Kevin Ruff, MD2, Cyril Varghese, MD2, Suryakanth Gurudu, MD2. P3677 - An Unusual Pulmonary Presentation of Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

