Tuesday Poster Session
Category: IBD
P3679 - Ustekinumab and Tofacitinib Combination Therapy: Success in a Difficult Case of Crohn’s Disease With Enteropathic Arthritis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Arvin Daneshmand, MD
University of Florida
Gainesville, FL
Presenting Author(s)
Award: Presidential Poster Award
Arvin Daneshmand, MD1, Diana N. Rodriguez, MD2, Steve Shen, MD1, Saroja Devi Rampertab, MD1, Ellen Zimmerman, MD1, Angela Pham, MD1, Naueen A. Chaudhry, MD1, Catalina Sanchez Alvarez, MD1
1University of Florida, Gainesville, FL; 2UF Health Shands Hospital, Gainesville, FL
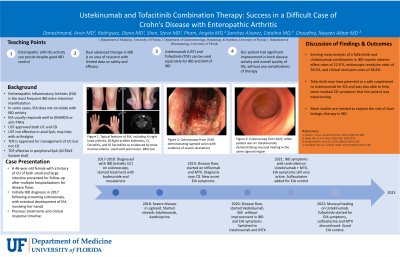
Introduction: Enteropathic Inflammatory Arthritis (EIA) is the most frequent extra-intestinal manifestation of Inflammatory Bowel Disease (IBD) [1]. The symptoms of polyarthritic EIA often correlate with IBD disease activity [2], although in some patients this may be asynchronous with management. Symptoms of peripheral polyarthritic EIA can be effectively managed with conventional Disease Modifying Agents (DMARDS) or anti-TNFα agents. For anti-TNFα non-responder patients, treatment options are limited. Ustekinumab (UST) is an effective agent for management of IBD [3], however its role in the treatment of EIA is less established [4]. Tofacitinib (TOF) is not approved for management of Crohn’s Disease (CD) [5], but has shown some promise in treatment of Axial EIA. Its role in management of peripheral EIA is not well-defined. Here we discuss a case of CD and polyarthritic EIA that was successfully treated with combination therapy of UST and TOF.
Case Description/Methods: A 46-year-old female with a history of uncomplicated CD presented for follow-up after multiple hospitalizations for disease flares. She had been trialed on multiple treatment regiments, including methotrexate (MTX), oral steroids, Adalimumab, Vedolizumab, and azathioprine with poor disease control. She eventually started on UST with clinical and endoscopic remission of CD.
Despite CD remission with UST, she continued to have active symptoms of peripheral EIA. Sulfasalazine and MTX were added without improvement, and she remained steroid dependent due to persistent severe arthralgias and poor quality of life. MTX was then discontinued and TOF was introduced for her joint symptoms. This brought rapid resolution of her arthralgias and further improvement in her GI symptoms. She was able to discontinue sulfasalazine and prednisone completely, with a drastic improvement in quality of life.
Discussion: Combination of advanced therapies for patient centered care is an evolving field in IBD, but most data is limited to case reports and retrospective studies [6]. Meta analysis of a TOF and UST combination in IBD reports adverse effect rates of 22.8 %, endoscopic remission rates of 38.5%, and clinical remission rates of 38.6% [10].
We present a unique case of UST and TOF combination therapy used in conjunction for management of CD and peripheral EIA, which is rarely reported in existing literature. TOF may have potential as a safe supplement to UST for EIA and was also able to help some residual CD symptoms that the patient was experiencing.
Disclosures:
Arvin Daneshmand, MD1, Diana N. Rodriguez, MD2, Steve Shen, MD1, Saroja Devi Rampertab, MD1, Ellen Zimmerman, MD1, Angela Pham, MD1, Naueen A. Chaudhry, MD1, Catalina Sanchez Alvarez, MD1. P3679 - Ustekinumab and Tofacitinib Combination Therapy: Success in a Difficult Case of Crohn’s Disease With Enteropathic Arthritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Arvin Daneshmand, MD1, Diana N. Rodriguez, MD2, Steve Shen, MD1, Saroja Devi Rampertab, MD1, Ellen Zimmerman, MD1, Angela Pham, MD1, Naueen A. Chaudhry, MD1, Catalina Sanchez Alvarez, MD1
1University of Florida, Gainesville, FL; 2UF Health Shands Hospital, Gainesville, FL
Introduction: Enteropathic Inflammatory Arthritis (EIA) is the most frequent extra-intestinal manifestation of Inflammatory Bowel Disease (IBD) [1]. The symptoms of polyarthritic EIA often correlate with IBD disease activity [2], although in some patients this may be asynchronous with management. Symptoms of peripheral polyarthritic EIA can be effectively managed with conventional Disease Modifying Agents (DMARDS) or anti-TNFα agents. For anti-TNFα non-responder patients, treatment options are limited. Ustekinumab (UST) is an effective agent for management of IBD [3], however its role in the treatment of EIA is less established [4]. Tofacitinib (TOF) is not approved for management of Crohn’s Disease (CD) [5], but has shown some promise in treatment of Axial EIA. Its role in management of peripheral EIA is not well-defined. Here we discuss a case of CD and polyarthritic EIA that was successfully treated with combination therapy of UST and TOF.
Case Description/Methods: A 46-year-old female with a history of uncomplicated CD presented for follow-up after multiple hospitalizations for disease flares. She had been trialed on multiple treatment regiments, including methotrexate (MTX), oral steroids, Adalimumab, Vedolizumab, and azathioprine with poor disease control. She eventually started on UST with clinical and endoscopic remission of CD.
Despite CD remission with UST, she continued to have active symptoms of peripheral EIA. Sulfasalazine and MTX were added without improvement, and she remained steroid dependent due to persistent severe arthralgias and poor quality of life. MTX was then discontinued and TOF was introduced for her joint symptoms. This brought rapid resolution of her arthralgias and further improvement in her GI symptoms. She was able to discontinue sulfasalazine and prednisone completely, with a drastic improvement in quality of life.
Discussion: Combination of advanced therapies for patient centered care is an evolving field in IBD, but most data is limited to case reports and retrospective studies [6]. Meta analysis of a TOF and UST combination in IBD reports adverse effect rates of 22.8 %, endoscopic remission rates of 38.5%, and clinical remission rates of 38.6% [10].
We present a unique case of UST and TOF combination therapy used in conjunction for management of CD and peripheral EIA, which is rarely reported in existing literature. TOF may have potential as a safe supplement to UST for EIA and was also able to help some residual CD symptoms that the patient was experiencing.
Disclosures:
Arvin Daneshmand indicated no relevant financial relationships.
Diana Rodriguez indicated no relevant financial relationships.
Steve Shen indicated no relevant financial relationships.
Saroja Devi Rampertab indicated no relevant financial relationships.
Ellen Zimmerman indicated no relevant financial relationships.
Angela Pham indicated no relevant financial relationships.
Naueen Chaudhry indicated no relevant financial relationships.
Catalina Sanchez Alvarez indicated no relevant financial relationships.
Arvin Daneshmand, MD1, Diana N. Rodriguez, MD2, Steve Shen, MD1, Saroja Devi Rampertab, MD1, Ellen Zimmerman, MD1, Angela Pham, MD1, Naueen A. Chaudhry, MD1, Catalina Sanchez Alvarez, MD1. P3679 - Ustekinumab and Tofacitinib Combination Therapy: Success in a Difficult Case of Crohn’s Disease With Enteropathic Arthritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

