Tuesday Poster Session
Category: IBD
P3680 - Microscopic to Macroscopic: A Case Highlighting Progression Along an Inflammatory Bowel Disease Spectrum
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Arvin Daneshmand, MD
University of Florida
Gainesville, FL
Presenting Author(s)
Arvin Daneshmand, MD1, Eugene Stolow, MD1, Charles Middleton, MD1, Christina Covelli, MD2, Lara Dakhoul, MD1
1University of Florida, Gainesville, FL; 2Orlando Health, Orlando, FL
Introduction: MC is an inflammatory colonic disease often predominant in female patients between 60 and 65 years of age. The diagnosis of MC requires a normal endoscopic evaluation but abnormal biopsies with evidence of either lymphocytic or collagenous colitis [1].
MC has significant symptom overlap with Inflammatory Bowel Diseases (IBD); however, diarrhea tends to be more watery than bloody with minimal abdominal pain compared to IBD [4]. There is also a histologic overlap between the two entities, such as crypt abnormalities and Paneth cell metaplasia. A small subset of patients have been reported to progress from MC to more severe forms of IBD such as Ulcerative Colitis (UC) or Crohn’s Disease (CD) [4]. Here we highlight one such case of MC progressing to UC, highlighting the importance of recognizing this potential clinical progression.
Case Description/Methods: A 69-year-old female was referred to our clinic for persistent watery diarrhea. She was diagnosed with collagenous colitis 7 years prior, and her diagnosis was biopsy-proven with a normal colonoscopy. Her diarrhea was refractory to budesonide therapy. Repeat colonoscopy showed normal endoscopic findings in the colon and the terminal ileum; however, random colon biopsies demonstrated chronic quiescent colitis with crypt dropout, basal lymphoplasmacytosis, and ganglion cells in the lamina propria (Figure 1A). This combination of clinical, endoscopic, and histopathological findings, particularly the absence of subepithelial collagen bands and intraepithelial lymphocytes seen in Microscopic Colitis (MC), prompted a new diagnosis of Ulcerative Colitis (UC).
The patient was treated with prednisone and Vedolizumab. A repeat colonoscopy with chromoendoscopy six months later revealed severe scarring with congestion throughout the colon. Targeted biopsies revealed multifocal areas of low-grade dysplasia throughout the colon. The patient subsequently underwent laparoscopic total proctocolectomy with end ileostomy.
Discussion: While exceedingly rare (< 1%), there is increasing evidence of the progression of MC to UC or Crohn’s Disease (CD) [5] The pathogenesis may be explained by a higher prevalence of Th1, Th2, and Tumor Necrosis Factor Alpha (TNF-alpha) lymphocyte subsets in patients who progress to UC compared to those with MC without disease progression [6]. The progression of MC to UC should be on the differential diagnosis when considering a patient whose symptoms remain refractory to conventional therapy, as has been highlighted by our case report.

Disclosures:
Arvin Daneshmand, MD1, Eugene Stolow, MD1, Charles Middleton, MD1, Christina Covelli, MD2, Lara Dakhoul, MD1. P3680 - Microscopic to Macroscopic: A Case Highlighting Progression Along an Inflammatory Bowel Disease Spectrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Florida, Gainesville, FL; 2Orlando Health, Orlando, FL
Introduction: MC is an inflammatory colonic disease often predominant in female patients between 60 and 65 years of age. The diagnosis of MC requires a normal endoscopic evaluation but abnormal biopsies with evidence of either lymphocytic or collagenous colitis [1].
MC has significant symptom overlap with Inflammatory Bowel Diseases (IBD); however, diarrhea tends to be more watery than bloody with minimal abdominal pain compared to IBD [4]. There is also a histologic overlap between the two entities, such as crypt abnormalities and Paneth cell metaplasia. A small subset of patients have been reported to progress from MC to more severe forms of IBD such as Ulcerative Colitis (UC) or Crohn’s Disease (CD) [4]. Here we highlight one such case of MC progressing to UC, highlighting the importance of recognizing this potential clinical progression.
Case Description/Methods: A 69-year-old female was referred to our clinic for persistent watery diarrhea. She was diagnosed with collagenous colitis 7 years prior, and her diagnosis was biopsy-proven with a normal colonoscopy. Her diarrhea was refractory to budesonide therapy. Repeat colonoscopy showed normal endoscopic findings in the colon and the terminal ileum; however, random colon biopsies demonstrated chronic quiescent colitis with crypt dropout, basal lymphoplasmacytosis, and ganglion cells in the lamina propria (Figure 1A). This combination of clinical, endoscopic, and histopathological findings, particularly the absence of subepithelial collagen bands and intraepithelial lymphocytes seen in Microscopic Colitis (MC), prompted a new diagnosis of Ulcerative Colitis (UC).
The patient was treated with prednisone and Vedolizumab. A repeat colonoscopy with chromoendoscopy six months later revealed severe scarring with congestion throughout the colon. Targeted biopsies revealed multifocal areas of low-grade dysplasia throughout the colon. The patient subsequently underwent laparoscopic total proctocolectomy with end ileostomy.
Discussion: While exceedingly rare (< 1%), there is increasing evidence of the progression of MC to UC or Crohn’s Disease (CD) [5] The pathogenesis may be explained by a higher prevalence of Th1, Th2, and Tumor Necrosis Factor Alpha (TNF-alpha) lymphocyte subsets in patients who progress to UC compared to those with MC without disease progression [6]. The progression of MC to UC should be on the differential diagnosis when considering a patient whose symptoms remain refractory to conventional therapy, as has been highlighted by our case report.

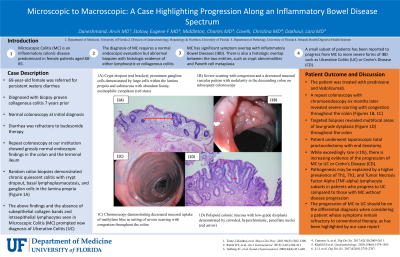
Figure: 1A) Crypt dropout (red bracket); prominent ganglion cells demonstrated by large cells within the lamina propria and submucosa with abundant foamy, eosinophilic cytoplasm (red stars)
(10x objective (100x magnification), H&E)
1B) Severe scarring with congestion and a decreased mucosal vascular pattern with nodularity in the descending colon on subsequent colonoscopy
1C) Chromoscopy demonstrating decreased mucosal uptake of methylene blue in setting of severe scarring with congestion throughout the colon
1D) Polypoid colonic mucosa with low-grade dysplasia demonstrated by crowded, hyperchromatic, pencillate nuclei (red arrow; 10x objective (100x magnification), H&E)
(10x objective (100x magnification), H&E)
1B) Severe scarring with congestion and a decreased mucosal vascular pattern with nodularity in the descending colon on subsequent colonoscopy
1C) Chromoscopy demonstrating decreased mucosal uptake of methylene blue in setting of severe scarring with congestion throughout the colon
1D) Polypoid colonic mucosa with low-grade dysplasia demonstrated by crowded, hyperchromatic, pencillate nuclei (red arrow; 10x objective (100x magnification), H&E)
Disclosures:
Arvin Daneshmand indicated no relevant financial relationships.
Eugene Stolow indicated no relevant financial relationships.
Charles Middleton indicated no relevant financial relationships.
Christina Covelli indicated no relevant financial relationships.
Lara Dakhoul indicated no relevant financial relationships.
Arvin Daneshmand, MD1, Eugene Stolow, MD1, Charles Middleton, MD1, Christina Covelli, MD2, Lara Dakhoul, MD1. P3680 - Microscopic to Macroscopic: A Case Highlighting Progression Along an Inflammatory Bowel Disease Spectrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
