Tuesday Poster Session
Category: IBD
P3683 - A Sigmoid Adeno-Endocrine Tumor in Ulcerative Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Chinmay Trivedi, MD
Hackensack Meridian Palisades Medical Center
North Bergen, NJ
Presenting Author(s)
Chinmay Trivedi, MD, Shawn Philip, DO, Nazir Ahmed, MD, John Sotiriadis, MD, PhD
Hackensack Meridian Palisades Medical Center, North Bergen, NJ
Introduction: The innate immune-mediated mucosal dysregulation and chronic mucosal inflammation associated with Inflammatory Bowel Disease (IBD) significantly increase the risk of colorectal cancer (CRC). Due to the differences in the pattern of gross presentation of IBD-associated dysplasia compared to the sporadic CRC occurring secondary to the adenoma-carcinoma sequence, IBD-associated dysplasias are more likely to be missed on standard endoscopic techniques. In addition to the higher risk of adenocarcinomas in IBD patients, there is an increased risk of neuroendocrine carcinomas.
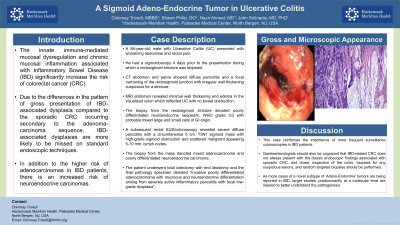
Case Description/Methods: A 58-year-old male with Ulcerative Colitis (UC) presented with worsening abdominal and rectal pain. He had a sigmoidoscopy 4 days prior to the presentation during which a rectosigmoid stricture was biopsied. CT abdomen and pelvis showed diffuse pancolitis and a focal narrowing of the rectosigmoid junction with irregular wall thickening suspicious for a stricture. MRI abdomen revealed minimal wall thickening and edema in the visualized colon which reflected UC with no bowel obstruction. The biopsy from the rectosigmoid stricture denoted poorly differentiated neuroendocrine neoplasm, WHO grade 3/3 with probable mixed large and small cells of GI origin. A subsequent rectal EUS/colonoscopy revealed severe diffuse pancolitis with a circumferential 5 cm. T3N1 sigmoid mass with high-grade sigmoid obstruction and scattered malignant appearing 5-10 mm. lymph nodes. The biopsy from the mass denoted mixed adenocarcinoma and poorly differentiated neuroendocrine carcinoma. The patient underwent total colectomy with end ileostomy and the final pathology specimen denoted “Invasive poorly differentiated adenocarcinoma with mucinous and neuroendocrine differentiation arising from severely active inflammatory pancolitis with focal low-grade dysplasia”.
Discussion: This case reinforces the importance of more frequent surveillance colonoscopies in IBD patients. Gastroenterologists should also be cognizant that IBD-related CRC does not always present with the classic endoscopic findings associated with sporadic CRC, and closer inspection of the colon, biopsies for any suspicious lesions, and random targeted biopsies should be performed. As more cases of a novel subtype of ‘Adeno-Endocrine’ tumors are being reported in IBD, larger studies, predominantly at a molecular level are needed to better understand the pathogenesis.

Disclosures:
Chinmay Trivedi, MD, Shawn Philip, DO, Nazir Ahmed, MD, John Sotiriadis, MD, PhD. P3683 - A Sigmoid Adeno-Endocrine Tumor in Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Hackensack Meridian Palisades Medical Center, North Bergen, NJ
Introduction: The innate immune-mediated mucosal dysregulation and chronic mucosal inflammation associated with Inflammatory Bowel Disease (IBD) significantly increase the risk of colorectal cancer (CRC). Due to the differences in the pattern of gross presentation of IBD-associated dysplasia compared to the sporadic CRC occurring secondary to the adenoma-carcinoma sequence, IBD-associated dysplasias are more likely to be missed on standard endoscopic techniques. In addition to the higher risk of adenocarcinomas in IBD patients, there is an increased risk of neuroendocrine carcinomas.
Case Description/Methods: A 58-year-old male with Ulcerative Colitis (UC) presented with worsening abdominal and rectal pain. He had a sigmoidoscopy 4 days prior to the presentation during which a rectosigmoid stricture was biopsied. CT abdomen and pelvis showed diffuse pancolitis and a focal narrowing of the rectosigmoid junction with irregular wall thickening suspicious for a stricture. MRI abdomen revealed minimal wall thickening and edema in the visualized colon which reflected UC with no bowel obstruction. The biopsy from the rectosigmoid stricture denoted poorly differentiated neuroendocrine neoplasm, WHO grade 3/3 with probable mixed large and small cells of GI origin. A subsequent rectal EUS/colonoscopy revealed severe diffuse pancolitis with a circumferential 5 cm. T3N1 sigmoid mass with high-grade sigmoid obstruction and scattered malignant appearing 5-10 mm. lymph nodes. The biopsy from the mass denoted mixed adenocarcinoma and poorly differentiated neuroendocrine carcinoma. The patient underwent total colectomy with end ileostomy and the final pathology specimen denoted “Invasive poorly differentiated adenocarcinoma with mucinous and neuroendocrine differentiation arising from severely active inflammatory pancolitis with focal low-grade dysplasia”.
Discussion: This case reinforces the importance of more frequent surveillance colonoscopies in IBD patients. Gastroenterologists should also be cognizant that IBD-related CRC does not always present with the classic endoscopic findings associated with sporadic CRC, and closer inspection of the colon, biopsies for any suspicious lesions, and random targeted biopsies should be performed. As more cases of a novel subtype of ‘Adeno-Endocrine’ tumors are being reported in IBD, larger studies, predominantly at a molecular level are needed to better understand the pathogenesis.

Figure: Gross and Microscopy Images of the Sigmoid Adenoendocrine tumor
Disclosures:
Chinmay Trivedi indicated no relevant financial relationships.
Shawn Philip indicated no relevant financial relationships.
Nazir Ahmed indicated no relevant financial relationships.
John Sotiriadis indicated no relevant financial relationships.
Chinmay Trivedi, MD, Shawn Philip, DO, Nazir Ahmed, MD, John Sotiriadis, MD, PhD. P3683 - A Sigmoid Adeno-Endocrine Tumor in Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
