Tuesday Poster Session
Category: IBD
P3684 - Successful Treatment of Rituximab-Induced Crohn’s Disease in a Patient with Rituximab-Dependent Optic Papillitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- XL
Xue Jing Li, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Xue Jing Li, MD, Rashmi Kumar, MD
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Rituximab (RTX) is a common therapy used in autoimmune and lymphoproliferative diseases. Development of RTX-induced Crohn’s disease (CD) has been reported previously, however, the exact mechanism of pathogenesis is unclear. There is also limited data on treatment. We found only one case report where ustekinumab (UST) was successfully used in the treatment of fistulizing CD induced by RTX. Here, we present a case of RTX-induced CD treated successfully with UST with long-term remission while continuing the RTX treatment.
Case Description/Methods: A 51-year-old Caucasian male was diagnosed with autoimmune optic papillitis after presenting with vision loss. Multiple sclerosis was ruled out following lumbar puncture/image/autoimmune workup. He initially underwent 6 rounds of plasma exchange and steroids, and was started on RTX by his neurologist and neuro-opthalmologist. Four years after being on RTX, he developed abdominal pain, diarrhea, 60lb unintentional weight loss. Pertinent labs were elevated CRP of 68, and low albumin 2.8.
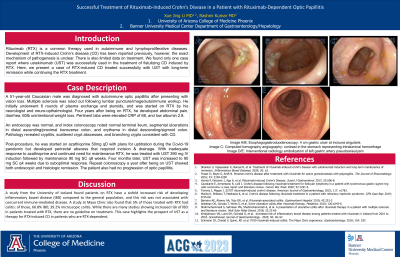
An endoscopy was normal, and index colonoscopy noted normal terminal ileum, segmental ulcerations in distal ascending/proximal transverse colon, and erythema in distal descending/sigmoid colon. Pathology revealed cryptitis, scattered crypt abscesses, and branching crypts consistent with CD.
Post-procedure, he was started on azathioprine 50mg qD with plans for uptitration during the Covid-19 pandemic but developed perirectal abscess that required incision & drainage. With inadequate response to azathioprine and continued need for maintenance RTX, he was treated with UST 390 mg IV induction followed by maintenance 90 mg SC q8 weeks. Four months later, UST was increased to 90 mg SC q4 weeks due to suboptimal response. Repeat colonoscopy a year after being on UST showed both endoscopic and histologic remission. The patient also had no progression of optic papillitis.
Discussion: A study from the University of Iceland found patients on RTX have a sixfold increased risk of developing inflammatory bowel disease (IBD) compared to the general population, and this risk was not associated with concurrent immune-mediated disease. A study at Mayo Clinic also found that 5% of those treated with RTX had colitis: of those, 60.8% IBD, 39.2% microscopic colitis. While there are many studies showing increased risk of IBD in patients treated with RTX, there are no guideline on treatment. This case highlights the prospect of UST as a therapy for RTX-induced CD in patients who are RTX-dependent.

Disclosures:
Xue Jing Li, MD, Rashmi Kumar, MD. P3684 - Successful Treatment of Rituximab-Induced Crohn’s Disease in a Patient with Rituximab-Dependent Optic Papillitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Rituximab (RTX) is a common therapy used in autoimmune and lymphoproliferative diseases. Development of RTX-induced Crohn’s disease (CD) has been reported previously, however, the exact mechanism of pathogenesis is unclear. There is also limited data on treatment. We found only one case report where ustekinumab (UST) was successfully used in the treatment of fistulizing CD induced by RTX. Here, we present a case of RTX-induced CD treated successfully with UST with long-term remission while continuing the RTX treatment.
Case Description/Methods: A 51-year-old Caucasian male was diagnosed with autoimmune optic papillitis after presenting with vision loss. Multiple sclerosis was ruled out following lumbar puncture/image/autoimmune workup. He initially underwent 6 rounds of plasma exchange and steroids, and was started on RTX by his neurologist and neuro-opthalmologist. Four years after being on RTX, he developed abdominal pain, diarrhea, 60lb unintentional weight loss. Pertinent labs were elevated CRP of 68, and low albumin 2.8.
An endoscopy was normal, and index colonoscopy noted normal terminal ileum, segmental ulcerations in distal ascending/proximal transverse colon, and erythema in distal descending/sigmoid colon. Pathology revealed cryptitis, scattered crypt abscesses, and branching crypts consistent with CD.
Post-procedure, he was started on azathioprine 50mg qD with plans for uptitration during the Covid-19 pandemic but developed perirectal abscess that required incision & drainage. With inadequate response to azathioprine and continued need for maintenance RTX, he was treated with UST 390 mg IV induction followed by maintenance 90 mg SC q8 weeks. Four months later, UST was increased to 90 mg SC q4 weeks due to suboptimal response. Repeat colonoscopy a year after being on UST showed both endoscopic and histologic remission. The patient also had no progression of optic papillitis.
Discussion: A study from the University of Iceland found patients on RTX have a sixfold increased risk of developing inflammatory bowel disease (IBD) compared to the general population, and this risk was not associated with concurrent immune-mediated disease. A study at Mayo Clinic also found that 5% of those treated with RTX had colitis: of those, 60.8% IBD, 39.2% microscopic colitis. While there are many studies showing increased risk of IBD in patients treated with RTX, there are no guideline on treatment. This case highlights the prospect of UST as a therapy for RTX-induced CD in patients who are RTX-dependent.

Figure: Image A/B: index colonoscopy with segmental ulcerations in proximal transverse colon (A), and erythema in sigmoid colon (B). Image C/D: follow-up colonoscopy a year after being on ustekinumab with endoscopic remission, as seen in transverse colon (C) and sigmoid colon (D)
Disclosures:
Xue Jing Li indicated no relevant financial relationships.
Rashmi Kumar indicated no relevant financial relationships.
Xue Jing Li, MD, Rashmi Kumar, MD. P3684 - Successful Treatment of Rituximab-Induced Crohn’s Disease in a Patient with Rituximab-Dependent Optic Papillitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
