Tuesday Poster Session
Category: IBD
P3686 - A Fatal Case of Bilateral Extremity Necrotizing Fasciitis in a Patient With Crohn's Disease on Biologic Therapy Presenting Initially as Anasarca
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sudheer Dhoop, MD
University of Toledo
Toledo, OH
Presenting Author(s)
Sudheer Dhoop, MD1, Sahithi Chinnam, DO1, Thomas Sodeman, MD2
1University of Toledo, Toledo, OH; 2University of Toledo Medical Center, Toledo, OH
Introduction: Necrotizing Fasciitis is a well documented complication of Crohn's Disease (CD) particularly in patients on biologic therapy. Typically the onset of the condition is rapidly progressive and leads to mortality without prompt surgical debridement.
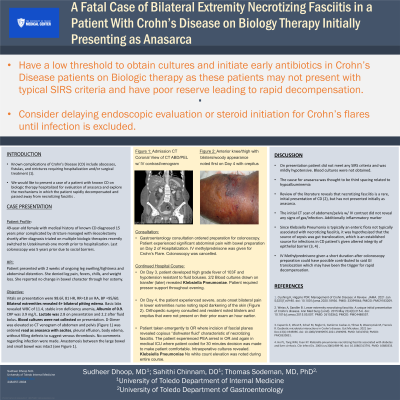
Case Description/Methods: A 49 year old female was admitted with two months of worsening of chronic, pitting lower extremity edema attributed to third-spacing with history of CD s/p Ileocolectomy for stricture at time of diagnosis treated with multiple biologic therapies recently switched to Ustekinumab one month prior. She had not undergone colonoscopy for >3 years due to social barriers. Vitals on presentation were 37.1F, 81 HR, RR=18 on RA, BP =85/50 deemed chronic. Basic labs revealed WBC of 18.6, stable iron deficiency anemia, Albumin of 0.9. Lactate was 2.8 on presentation and 2.2 after fluid bolus. D-Dimer was elevated so CT venogram of abdomen and pelvis (figure 1) was ordered revealing no signs of thrombosis of infection. ECHO was unremarkable. The patient had no clinical signs of Crohn's Flare. GI was consulted and the decision was made to pursue colonoscopy to assess disease burden. The colonoscopy preparation led to GI distress so the patient was given IV methylprednisolone and developed tachycardia and new leg pain and swelling. On day 3, her hypotension was resistant to fluids so she was transferred to the ICU where blood cultures were drawn and she was started on broad spectrum antibiotics/pressor support. On day 4 of hospitalization, the patient's blood cultures grew 2/2 Klebsiella Pneumoniae and Orthopedic Surgery was consulted given woody appearance of the extremities with rapidly progressive pain. OR incision of fascial planes revealed copious dishwater fluid characteristic of necrotizing fasciitis. The patient experienced PEA arrest in OR and again on the medical ICU and passed away. Intraoperative cultures revealed Klebsiella Pneumoniae.
Discussion: A lower threshold for septic evaluation and treatment in CD on presentation should be employed. The localizing source of infection was not immediately obvious here as the patient's leg edema was ongoing for a month and dedicated CT imaging did not reveal signs of infection. It is unclear what led to necrotizing fasciitis of the superimposed edematous tissue, but IV steroid treatment may have precipitated the patient's decline. Necrotizing fasciitis should be on the differential for increasing leg edema in CD patient's given their immunosuppressed state and potential for rapid decline.

Disclosures:
Sudheer Dhoop, MD1, Sahithi Chinnam, DO1, Thomas Sodeman, MD2. P3686 - A Fatal Case of Bilateral Extremity Necrotizing Fasciitis in a Patient With Crohn's Disease on Biologic Therapy Presenting Initially as Anasarca, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Toledo, Toledo, OH; 2University of Toledo Medical Center, Toledo, OH
Introduction: Necrotizing Fasciitis is a well documented complication of Crohn's Disease (CD) particularly in patients on biologic therapy. Typically the onset of the condition is rapidly progressive and leads to mortality without prompt surgical debridement.
Case Description/Methods: A 49 year old female was admitted with two months of worsening of chronic, pitting lower extremity edema attributed to third-spacing with history of CD s/p Ileocolectomy for stricture at time of diagnosis treated with multiple biologic therapies recently switched to Ustekinumab one month prior. She had not undergone colonoscopy for >3 years due to social barriers. Vitals on presentation were 37.1F, 81 HR, RR=18 on RA, BP =85/50 deemed chronic. Basic labs revealed WBC of 18.6, stable iron deficiency anemia, Albumin of 0.9. Lactate was 2.8 on presentation and 2.2 after fluid bolus. D-Dimer was elevated so CT venogram of abdomen and pelvis (figure 1) was ordered revealing no signs of thrombosis of infection. ECHO was unremarkable. The patient had no clinical signs of Crohn's Flare. GI was consulted and the decision was made to pursue colonoscopy to assess disease burden. The colonoscopy preparation led to GI distress so the patient was given IV methylprednisolone and developed tachycardia and new leg pain and swelling. On day 3, her hypotension was resistant to fluids so she was transferred to the ICU where blood cultures were drawn and she was started on broad spectrum antibiotics/pressor support. On day 4 of hospitalization, the patient's blood cultures grew 2/2 Klebsiella Pneumoniae and Orthopedic Surgery was consulted given woody appearance of the extremities with rapidly progressive pain. OR incision of fascial planes revealed copious dishwater fluid characteristic of necrotizing fasciitis. The patient experienced PEA arrest in OR and again on the medical ICU and passed away. Intraoperative cultures revealed Klebsiella Pneumoniae.
Discussion: A lower threshold for septic evaluation and treatment in CD on presentation should be employed. The localizing source of infection was not immediately obvious here as the patient's leg edema was ongoing for a month and dedicated CT imaging did not reveal signs of infection. It is unclear what led to necrotizing fasciitis of the superimposed edematous tissue, but IV steroid treatment may have precipitated the patient's decline. Necrotizing fasciitis should be on the differential for increasing leg edema in CD patient's given their immunosuppressed state and potential for rapid decline.

Figure: Image 1: Anasarca with ascites and pleural effusions and body wall edema.
Significant features of active inflammatory bowel disease with an intact anastomosis in the right flank
No drainable fluid collections. No obstruction.
There is hepatic steatosis identified.
There is no evidence of venous thrombosis in the lower limbs IVC or the portal venous system
Significant features of active inflammatory bowel disease with an intact anastomosis in the right flank
No drainable fluid collections. No obstruction.
There is hepatic steatosis identified.
There is no evidence of venous thrombosis in the lower limbs IVC or the portal venous system
Disclosures:
Sudheer Dhoop indicated no relevant financial relationships.
Sahithi Chinnam indicated no relevant financial relationships.
Thomas Sodeman indicated no relevant financial relationships.
Sudheer Dhoop, MD1, Sahithi Chinnam, DO1, Thomas Sodeman, MD2. P3686 - A Fatal Case of Bilateral Extremity Necrotizing Fasciitis in a Patient With Crohn's Disease on Biologic Therapy Presenting Initially as Anasarca, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
