Tuesday Poster Session
Category: IBD
P3688 - Continuation of Anti-Tumor Necrosis Factor-A Therapy in Anti-TNF-Induced Autoimmune Hepatitis – A Case Series
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sang Hee K. Choi, MD
Scripps Clinic/Scripps Green Hospital
La Jolla, CA
Presenting Author(s)
Sang Hee K. Choi, MD1, Lawrence Ku, MD2, Ashwini Mulgaonkar, MD2, Rebecca Matro, MD2, Mazer Ally, MD3, Melissa J. Ferrari, PA-C, MPAS4, Gauree G. Konijeti, MD, MPH2
1Scripps Clinic/Scripps Green Hospital, La Jolla, CA; 2Scripps Clinic, La Jolla, CA; 3Scripps Clinic, Oceanside, CA; 4Scripps Clinic Medical Group, La Jolla, CA
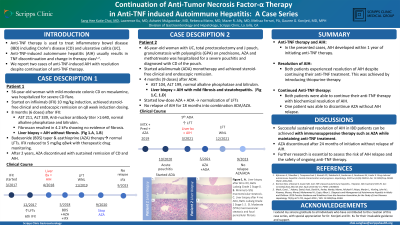
Introduction: Anti-TNF therapy is commonly used to treat inflammatory bowel disease (IBD) including Crohn’s disease (CD) and ulcerative colitis (UC). Anti-TNF-induced autoimmune hepatitis (AIH) usually results in TNF discontinuation and change in therapy class. We report two cases of anti-TNF-induced AIH with resolution despite continuation of anti-TNF therapy.
Case Description/Methods: Patient 1, a 56-year-old woman with mild-moderate colonic CD on mesalamine, was hospitalized for severe CD flare. While admitted she started infliximab (IFX) 10 mg/kg induction with a prednisone taper. She achieved steroid-free clinical and endoscopic remission on q8 week induction dosing. Liver function tests (LFTs) after 8 months were elevated 6-7 upper limit of normal (ULN) (Table 1). Anti-nuclear antibody titer was >1:640. Liver biopsy revealed AIH without fibrosis. Budesonide taper and azathioprine (AZA) therapy normalized LFTs. IFX was reduced to 5 mg/kg q8wk with therapeutic drug monitoring. AZA was discontinued after 2 years of stable AIH and CD remission, with sustained remission of CD (SESCD 0) and AIH (normal LFTs with aspartate aminotransferase (AST) 30-40 U/L).
Patient 2, a 46-year-old woman with UC for 20 years, total proctocolectomy and J pouch, granulomatosis with polyangiitis (GPA). Previous therapies for GPA included corticosteroids, AZA and methotrexate, with variable bowel habits during this time. She was hospitalized for severe pouchitis and diagnosed with CD of the pouch. Her pouchitis responded to antibiotics. Following multidisciplinary discussion, she started adalimumab (ADA) monotherapy and achieved steroid-free clinical and endoscopic remission. She developed a perianal abscess on antibiotics and required drainage. LFTs after 4 months on ADA were 3-4 ULN. Liver biopsy showed AIH with mild fibrosis and steatohepatitis. She started low-dose AZA with normalization of LFTs while continuing ADA.
Discussion: We present 2 patients who continued anti-TNF despite development of anti-TNF-induced AIH within a year of starting therapy. Both had mild AIH and responded to AZA while continuing anti-TNF therapy. To date, one patient has discontinued AZA while continuing anti-TNF without relapse of AIH. AIH severity is comparable to other published cases of TNF-induced AIH, with resolution of AIH after anti-TNF withdrawal and concomitant corticosteroid therapy. There is limited data on relapse risk while continuing anti-TNF; close monitoring is needed. Future studies examining long-term benefits and risks are needed.
Disclosures:
Sang Hee K. Choi, MD1, Lawrence Ku, MD2, Ashwini Mulgaonkar, MD2, Rebecca Matro, MD2, Mazer Ally, MD3, Melissa J. Ferrari, PA-C, MPAS4, Gauree G. Konijeti, MD, MPH2. P3688 - Continuation of Anti-Tumor Necrosis Factor-A Therapy in Anti-TNF-Induced Autoimmune Hepatitis – A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Scripps Clinic/Scripps Green Hospital, La Jolla, CA; 2Scripps Clinic, La Jolla, CA; 3Scripps Clinic, Oceanside, CA; 4Scripps Clinic Medical Group, La Jolla, CA
Introduction: Anti-TNF therapy is commonly used to treat inflammatory bowel disease (IBD) including Crohn’s disease (CD) and ulcerative colitis (UC). Anti-TNF-induced autoimmune hepatitis (AIH) usually results in TNF discontinuation and change in therapy class. We report two cases of anti-TNF-induced AIH with resolution despite continuation of anti-TNF therapy.
Case Description/Methods: Patient 1, a 56-year-old woman with mild-moderate colonic CD on mesalamine, was hospitalized for severe CD flare. While admitted she started infliximab (IFX) 10 mg/kg induction with a prednisone taper. She achieved steroid-free clinical and endoscopic remission on q8 week induction dosing. Liver function tests (LFTs) after 8 months were elevated 6-7 upper limit of normal (ULN) (Table 1). Anti-nuclear antibody titer was >1:640. Liver biopsy revealed AIH without fibrosis. Budesonide taper and azathioprine (AZA) therapy normalized LFTs. IFX was reduced to 5 mg/kg q8wk with therapeutic drug monitoring. AZA was discontinued after 2 years of stable AIH and CD remission, with sustained remission of CD (SESCD 0) and AIH (normal LFTs with aspartate aminotransferase (AST) 30-40 U/L).
Patient 2, a 46-year-old woman with UC for 20 years, total proctocolectomy and J pouch, granulomatosis with polyangiitis (GPA). Previous therapies for GPA included corticosteroids, AZA and methotrexate, with variable bowel habits during this time. She was hospitalized for severe pouchitis and diagnosed with CD of the pouch. Her pouchitis responded to antibiotics. Following multidisciplinary discussion, she started adalimumab (ADA) monotherapy and achieved steroid-free clinical and endoscopic remission. She developed a perianal abscess on antibiotics and required drainage. LFTs after 4 months on ADA were 3-4 ULN. Liver biopsy showed AIH with mild fibrosis and steatohepatitis. She started low-dose AZA with normalization of LFTs while continuing ADA.
Discussion: We present 2 patients who continued anti-TNF despite development of anti-TNF-induced AIH within a year of starting therapy. Both had mild AIH and responded to AZA while continuing anti-TNF therapy. To date, one patient has discontinued AZA while continuing anti-TNF without relapse of AIH. AIH severity is comparable to other published cases of TNF-induced AIH, with resolution of AIH after anti-TNF withdrawal and concomitant corticosteroid therapy. There is limited data on relapse risk while continuing anti-TNF; close monitoring is needed. Future studies examining long-term benefits and risks are needed.
Disclosures:
Sang Hee Choi indicated no relevant financial relationships.
Lawrence Ku indicated no relevant financial relationships.
Ashwini Mulgaonkar indicated no relevant financial relationships.
Rebecca Matro: Abbvie – Speakers Bureau.
Mazer Ally: Abbvie – Speakers Bureau. Lilly – Advisory Committee/Board Member.
Melissa Ferrari: Abbvie – Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member.
Gauree Konijeti: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Sang Hee K. Choi, MD1, Lawrence Ku, MD2, Ashwini Mulgaonkar, MD2, Rebecca Matro, MD2, Mazer Ally, MD3, Melissa J. Ferrari, PA-C, MPAS4, Gauree G. Konijeti, MD, MPH2. P3688 - Continuation of Anti-Tumor Necrosis Factor-A Therapy in Anti-TNF-Induced Autoimmune Hepatitis – A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

