Tuesday Poster Session
Category: Interventional Endoscopy
P3690 - Impact of the COVID-19 Pandemic on Patients Undergoing ERCP: A Retrospective Single Center Chart Review Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kassem Barada, MD
American University of Beirut
Beirut, Beyrouth, Lebanon
Presenting Author(s)
Mohamad Ali Ibrahim, MD1, Maria Chalfoun, MD1, Ahmad Moussawi, MD1, Ali Hajj Ali, 1, Lynn Kobeissi, 1, Abbas Hammoud, 1, Ali Elhadi Zreik, MD1, Chantal Rizk, MD1, Kassem Barada, MD2, Yasser Shaib, MD, MPH1
1American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon; 2American University of Beirut, Beirut, Beyrouth, Lebanon
Introduction: The COVID-19 outbreak significantly impacted healthcare systems disrupting routine patient care worldwide. We aim to determine the COVID-19 pandemic's impact on the indications, outcomes, and adverse events of endoscopic retrograde cholangiopancreatography (ERCP) procedures.
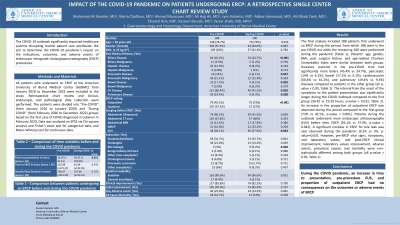
Methods: All patients who underwent an ERCP at the American University of Beirut Medical Center (AUBMC) from January 2018 to December 2022 were included in the study. Retrospective chart review and clinical, endoscopic, and pathological data collection were performed. The patients were divided into “Pre-COVID” (from January 2018 to January 2020) and “During COVID” (from February 2020 to December 2022) groups based on the first case of COVID diagnosed in Lebanon in February 2020. Data was analyzed on SPSS via Chi-square analysis and Fisher’s exact test for categorical data, and Mann-Whitney test for continuous data.
Results: The final analysis included 288 patients that underwent an ERCP during this period, from which 188 were in the pre-COVID era while the remaining 100 were performed during the pandemic (Table 1). Patients’ age, gender, BMI, past surgical history, and age-related Charlson Comorbidity Index were similar between both groups. However, patients in the pre-COVID time had significantly more biliary (45.4% vs 24.7%), pancreatic (14% vs 6.1%), bowel (17.2% vs 4.1%), and cardiovascular (60.4% vs 41.2%) diseases compared to patients in the other group (all p-value < 0.05). The interval from the onset of the symptoms to the patient presentation was significantly longer during the COVID outbreak compared to the first group (39.42 vs 19.29 hours, p-value = 0.012). An increase in the proportion of outpatient ERCP was observed during this period compared to the first group (73% vs 42.5%, p-value < 0.001). Patients during the outbreak underwent more endoscopic ultrasonography (EUS) before their ERCP (26.1% vs 37.9%, p-value = 0.042). A significant increase in ERCP for bile leak was also observed during the pandemic (9.2% vs 3%, p-value=0.03) However, pre-ERCP vital signs, symptoms, and laboratory values, and post-ERCP clinical improvement, laboratory values improvement, adverse events, procedure repeat, and mortality were non-statistically different among both groups (all p-value > 0.05).
Discussion: During the COVID pandemic, an increase in time to presentation, pre-procedure EUS, and proportion of outpatient ERCP had no consequences on the outcomes or adverse events of ERCP.
Disclosures:
Mohamad Ali Ibrahim, MD1, Maria Chalfoun, MD1, Ahmad Moussawi, MD1, Ali Hajj Ali, 1, Lynn Kobeissi, 1, Abbas Hammoud, 1, Ali Elhadi Zreik, MD1, Chantal Rizk, MD1, Kassem Barada, MD2, Yasser Shaib, MD, MPH1. P3690 - Impact of the COVID-19 Pandemic on Patients Undergoing ERCP: A Retrospective Single Center Chart Review Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon; 2American University of Beirut, Beirut, Beyrouth, Lebanon
Introduction: The COVID-19 outbreak significantly impacted healthcare systems disrupting routine patient care worldwide. We aim to determine the COVID-19 pandemic's impact on the indications, outcomes, and adverse events of endoscopic retrograde cholangiopancreatography (ERCP) procedures.
Methods: All patients who underwent an ERCP at the American University of Beirut Medical Center (AUBMC) from January 2018 to December 2022 were included in the study. Retrospective chart review and clinical, endoscopic, and pathological data collection were performed. The patients were divided into “Pre-COVID” (from January 2018 to January 2020) and “During COVID” (from February 2020 to December 2022) groups based on the first case of COVID diagnosed in Lebanon in February 2020. Data was analyzed on SPSS via Chi-square analysis and Fisher’s exact test for categorical data, and Mann-Whitney test for continuous data.
Results: The final analysis included 288 patients that underwent an ERCP during this period, from which 188 were in the pre-COVID era while the remaining 100 were performed during the pandemic (Table 1). Patients’ age, gender, BMI, past surgical history, and age-related Charlson Comorbidity Index were similar between both groups. However, patients in the pre-COVID time had significantly more biliary (45.4% vs 24.7%), pancreatic (14% vs 6.1%), bowel (17.2% vs 4.1%), and cardiovascular (60.4% vs 41.2%) diseases compared to patients in the other group (all p-value < 0.05). The interval from the onset of the symptoms to the patient presentation was significantly longer during the COVID outbreak compared to the first group (39.42 vs 19.29 hours, p-value = 0.012). An increase in the proportion of outpatient ERCP was observed during this period compared to the first group (73% vs 42.5%, p-value < 0.001). Patients during the outbreak underwent more endoscopic ultrasonography (EUS) before their ERCP (26.1% vs 37.9%, p-value = 0.042). A significant increase in ERCP for bile leak was also observed during the pandemic (9.2% vs 3%, p-value=0.03) However, pre-ERCP vital signs, symptoms, and laboratory values, and post-ERCP clinical improvement, laboratory values improvement, adverse events, procedure repeat, and mortality were non-statistically different among both groups (all p-value > 0.05).
Discussion: During the COVID pandemic, an increase in time to presentation, pre-procedure EUS, and proportion of outpatient ERCP had no consequences on the outcomes or adverse events of ERCP.
Disclosures:
Mohamad Ali Ibrahim indicated no relevant financial relationships.
Maria Chalfoun indicated no relevant financial relationships.
Ahmad Moussawi indicated no relevant financial relationships.
Ali Hajj Ali indicated no relevant financial relationships.
Lynn Kobeissi indicated no relevant financial relationships.
Abbas Hammoud indicated no relevant financial relationships.
Ali Elhadi Zreik indicated no relevant financial relationships.
Chantal Rizk indicated no relevant financial relationships.
Kassem Barada indicated no relevant financial relationships.
Yasser Shaib indicated no relevant financial relationships.
Mohamad Ali Ibrahim, MD1, Maria Chalfoun, MD1, Ahmad Moussawi, MD1, Ali Hajj Ali, 1, Lynn Kobeissi, 1, Abbas Hammoud, 1, Ali Elhadi Zreik, MD1, Chantal Rizk, MD1, Kassem Barada, MD2, Yasser Shaib, MD, MPH1. P3690 - Impact of the COVID-19 Pandemic on Patients Undergoing ERCP: A Retrospective Single Center Chart Review Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
