Tuesday Poster Session
Category: Interventional Endoscopy
P3693 - Impact of Endoscopic Compared to Percutaneous Gallbladder Drainage for Patients With Acute Cholecystitis in Hospitalized Patients in the US
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Muhammad Haseeb, MD
Brigham and Women's Hospital
Pittsburgh, PA
Presenting Author(s)
Muhammad Haseeb, MD1, Maham Waqar, MBBS2, Sakina Abbas, 3, Muhammad Kamal, MD4, Anum Khakwani, MBBS, FCPS5, Umar Hayat, MD6, Fnu Faheela, MBBS5, Zubair Khan, MD7, Sultan Mahmood, MD8
1Brigham and Women's Hospital, Boston, MA; 2King Edward Medical University, Boston, MA; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Essen Health Care System, New York, NY; 5Nishtar Medical University, Multan, Punjab, Pakistan; 6Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 7Mercy Clinic, Poland, OH; 8Beth Israel Deaconess Medical Center, Boston, MA
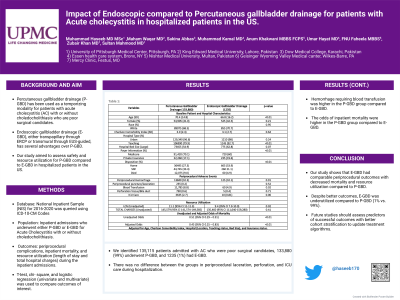
Introduction: Percutaneous gallbladder drainage (P-GBD) has been used as a temporizing modality for patients with acute cholecystitis (AC) with or without choledocholithiasis who are poor surgical candidates. However, there are several disadvantages despite the technical ease of the procedure. Endoscopic gallbladder drainage (E-GBD), either transpapillary through ERCP or transmural through EUS-guided, has several advantages over P-GBD. Our study aimed to assess safety and resource utilization for P-GBD compared to E-GBD in hospitalized patients in the US.
Methods: National Inpatient Sample (NIS) for 2016-2020 was queried using ICD-10-CM Codes to identify a cohort of inpatient admissions who underwent either P-GBD or E-GBD for AC with or without choledocholithiasis. A weighted sample was used to get baseline characteristics, periprocedural complications, inpatient mortality, and resource utilization (length of stay and total hospital charges) during the inpatient admissions. T-test, chi-square, and logistic regression (univariate and multivariate) was used to compare outcomes of interest.
Results: We identified 135,115 patients admitted with AC who were poor surgical candidates, 133,880 (99%) underwent P-GBD, and 1235 (1%) had E-GBD. Patients with P-GBD were older; however, other baseline characteristics and comorbidities were comparable between the two groups. (Charlson comorbidity index: 3 vs. 3.1). There was no difference between the groups in periprocedural laceration, perforation, and ICU care during hospitalization. Hemorrhage requiring blood transfusion was higher in the P-GBD group compared to E-GBD. The odds of inpatient mortality were higher in the P-GBD group compared to E-GBD in the unadjusted and adjusted model. (p-value < 0.01; Table 1).
Discussion: Our study shows that E-GBD had comparable periprocedural outcomes with decreased mortality and resource utilization compared to P-GBD. However, despite better outcomes, E-GBD was underutilized compared to P-GBD (1% vs. 99%). Future studies should assess predictors of successful outcomes with better cohort stratification to update treatment algorithms.
Disclosures:
Muhammad Haseeb, MD1, Maham Waqar, MBBS2, Sakina Abbas, 3, Muhammad Kamal, MD4, Anum Khakwani, MBBS, FCPS5, Umar Hayat, MD6, Fnu Faheela, MBBS5, Zubair Khan, MD7, Sultan Mahmood, MD8. P3693 - Impact of Endoscopic Compared to Percutaneous Gallbladder Drainage for Patients With Acute Cholecystitis in Hospitalized Patients in the US, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2King Edward Medical University, Boston, MA; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Essen Health Care System, New York, NY; 5Nishtar Medical University, Multan, Punjab, Pakistan; 6Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 7Mercy Clinic, Poland, OH; 8Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Percutaneous gallbladder drainage (P-GBD) has been used as a temporizing modality for patients with acute cholecystitis (AC) with or without choledocholithiasis who are poor surgical candidates. However, there are several disadvantages despite the technical ease of the procedure. Endoscopic gallbladder drainage (E-GBD), either transpapillary through ERCP or transmural through EUS-guided, has several advantages over P-GBD. Our study aimed to assess safety and resource utilization for P-GBD compared to E-GBD in hospitalized patients in the US.
Methods: National Inpatient Sample (NIS) for 2016-2020 was queried using ICD-10-CM Codes to identify a cohort of inpatient admissions who underwent either P-GBD or E-GBD for AC with or without choledocholithiasis. A weighted sample was used to get baseline characteristics, periprocedural complications, inpatient mortality, and resource utilization (length of stay and total hospital charges) during the inpatient admissions. T-test, chi-square, and logistic regression (univariate and multivariate) was used to compare outcomes of interest.
Results: We identified 135,115 patients admitted with AC who were poor surgical candidates, 133,880 (99%) underwent P-GBD, and 1235 (1%) had E-GBD. Patients with P-GBD were older; however, other baseline characteristics and comorbidities were comparable between the two groups. (Charlson comorbidity index: 3 vs. 3.1). There was no difference between the groups in periprocedural laceration, perforation, and ICU care during hospitalization. Hemorrhage requiring blood transfusion was higher in the P-GBD group compared to E-GBD. The odds of inpatient mortality were higher in the P-GBD group compared to E-GBD in the unadjusted and adjusted model. (p-value < 0.01; Table 1).
Discussion: Our study shows that E-GBD had comparable periprocedural outcomes with decreased mortality and resource utilization compared to P-GBD. However, despite better outcomes, E-GBD was underutilized compared to P-GBD (1% vs. 99%). Future studies should assess predictors of successful outcomes with better cohort stratification to update treatment algorithms.
Disclosures:
Muhammad Haseeb indicated no relevant financial relationships.
Maham Waqar indicated no relevant financial relationships.
Sakina Abbas indicated no relevant financial relationships.
Muhammad Kamal indicated no relevant financial relationships.
Anum Khakwani indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Fnu Faheela indicated no relevant financial relationships.
Zubair Khan indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Muhammad Haseeb, MD1, Maham Waqar, MBBS2, Sakina Abbas, 3, Muhammad Kamal, MD4, Anum Khakwani, MBBS, FCPS5, Umar Hayat, MD6, Fnu Faheela, MBBS5, Zubair Khan, MD7, Sultan Mahmood, MD8. P3693 - Impact of Endoscopic Compared to Percutaneous Gallbladder Drainage for Patients With Acute Cholecystitis in Hospitalized Patients in the US, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
