Tuesday Poster Session
Category: Interventional Endoscopy
P3698 - Outcomes of Endoscopic Submucosal Dissection for Distal Rectal Lesions Within 2 Cm of the Dentate Line – A Multicenter Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Talia F. Malik, MD
Chicago Medical School at Rosalind Franklin University of Medicine and Science
North Chicago, IL
Presenting Author(s)
Talia F.. Malik, MD1, Aqsa Khan, MD2, Harishankar Gopakumar, MD3, Dushyant Singh. Dahiya, MD4, Ishaan Vohra, MD3, Christina Zelt, BSN, RN2, Ashley Rumple, RN, BSN2, Antonio Mendoza-Ladd, MD5, Abdul Aziz. Aadam, MD6, Ahmed Saeed, MD7, Mohamed O. Othman, MD8, Suchapa Arayakarnkul, MD9, Saowanee Ngamruengphong, MD10, Amit Bhatt, MD11, Dennis Yang, MD12, Mariajose Rojas DeLeon, MD2, Peter V.. Draganov, MD13, Neil R.. Sharma, MD14
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 2Parkview Health, Fort Wayne, IN; 3University of Illinois, Peoria, IL; 4University of Kansas School of Medicine, Kansas City, KS; 5University of California Davis Health, Sacramento, CA; 6Northwestern University, Chicago, IL; 7Kansas City Gastroenterology and Hepatology, Kansas City, MO; 8Baylor College of Medicine, Houston, TX; 9Johns Hopkins University School of Medicine, Baltimore, MD; 10Johns Hopkins University School of Medicine, Batimore, MD; 11Cleveland Clinic, Cleveland, OH; 12AdventHealth, Orlando, FL; 13University of Florida, Gainesville, FL; 14Parkview Cancer Institue, Fort Wayne, IN
Introduction: Endoscopic submucosal dissection (ESD) is technically challenging for resection of distal rectal lesions located close to the dentate line due to various anatomical factors. It is known to be associated with an increased risk of incomplete resection and adverse events based on case series originating from Asian and European centers. However, compared to transanal resection performed by colorectal surgeons where the devices are limited by anatomy and stabilization, ESD provides advantages for these distal resections. We conducted the first multicenter study in North America studying the efficacy and safety of ESD for resection of distal rectal lesions within 2 cm of the dentate line.
Methods: This was a multicenter retrospective study of patients with distal rectal lesions located within 2 cm of the dentate line who underwent ESD between 2015-2023. The primary outcomes were rate of R0 resection and en bloc resection. Technical success was defined as complete macroscopic resection – R0 Resection. Additional outcomes measured were rate of adverse events including bleeding, perforation, need for hospitalization, and other procedure-related adverse events. Data was analyzed using descriptive statistics.
Results: Preliminary analysis from our study included a total of 108 patients across nine institutions. 51.9% of the patients were female and the mean age was 61.4 years (Table 1). The average lesion size was 43.9 mm.
The rate of R0 resection was 82.9%, (n=87), en bloc resection rate was 95.2% (n=99) and technical success was 100 % (n=108). The rate of overall adverse events was 7.5% (n=8). There were five cases of bleeding managed with Argon Plasma Coagulation and hemostatic clips. There were two cases of perforation and one case of postprocedural infection. Post-procedural infection was treated with intravenous antibiotics. Hospitalization was required for 30.6% (n=33) of the patients. The majority of hospitalizations were for observation (90.9%, n=30).
Discussion: Based on our preliminary data, ESD is safe and effective for resection of distal rectal lesions within 2 cm of the dentate line with a high rate of en bloc and R0 resection. Additional data from other centers is pending which will validate our findings. ESD may offer an excellent option for distal rectal lesions where transanal resection from colorectal surgery has technical limitations.

Disclosures:
Talia F.. Malik, MD1, Aqsa Khan, MD2, Harishankar Gopakumar, MD3, Dushyant Singh. Dahiya, MD4, Ishaan Vohra, MD3, Christina Zelt, BSN, RN2, Ashley Rumple, RN, BSN2, Antonio Mendoza-Ladd, MD5, Abdul Aziz. Aadam, MD6, Ahmed Saeed, MD7, Mohamed O. Othman, MD8, Suchapa Arayakarnkul, MD9, Saowanee Ngamruengphong, MD10, Amit Bhatt, MD11, Dennis Yang, MD12, Mariajose Rojas DeLeon, MD2, Peter V.. Draganov, MD13, Neil R.. Sharma, MD14. P3698 - Outcomes of Endoscopic Submucosal Dissection for Distal Rectal Lesions Within 2 Cm of the Dentate Line – A Multicenter Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 2Parkview Health, Fort Wayne, IN; 3University of Illinois, Peoria, IL; 4University of Kansas School of Medicine, Kansas City, KS; 5University of California Davis Health, Sacramento, CA; 6Northwestern University, Chicago, IL; 7Kansas City Gastroenterology and Hepatology, Kansas City, MO; 8Baylor College of Medicine, Houston, TX; 9Johns Hopkins University School of Medicine, Baltimore, MD; 10Johns Hopkins University School of Medicine, Batimore, MD; 11Cleveland Clinic, Cleveland, OH; 12AdventHealth, Orlando, FL; 13University of Florida, Gainesville, FL; 14Parkview Cancer Institue, Fort Wayne, IN
Introduction: Endoscopic submucosal dissection (ESD) is technically challenging for resection of distal rectal lesions located close to the dentate line due to various anatomical factors. It is known to be associated with an increased risk of incomplete resection and adverse events based on case series originating from Asian and European centers. However, compared to transanal resection performed by colorectal surgeons where the devices are limited by anatomy and stabilization, ESD provides advantages for these distal resections. We conducted the first multicenter study in North America studying the efficacy and safety of ESD for resection of distal rectal lesions within 2 cm of the dentate line.
Methods: This was a multicenter retrospective study of patients with distal rectal lesions located within 2 cm of the dentate line who underwent ESD between 2015-2023. The primary outcomes were rate of R0 resection and en bloc resection. Technical success was defined as complete macroscopic resection – R0 Resection. Additional outcomes measured were rate of adverse events including bleeding, perforation, need for hospitalization, and other procedure-related adverse events. Data was analyzed using descriptive statistics.
Results: Preliminary analysis from our study included a total of 108 patients across nine institutions. 51.9% of the patients were female and the mean age was 61.4 years (Table 1). The average lesion size was 43.9 mm.
The rate of R0 resection was 82.9%, (n=87), en bloc resection rate was 95.2% (n=99) and technical success was 100 % (n=108). The rate of overall adverse events was 7.5% (n=8). There were five cases of bleeding managed with Argon Plasma Coagulation and hemostatic clips. There were two cases of perforation and one case of postprocedural infection. Post-procedural infection was treated with intravenous antibiotics. Hospitalization was required for 30.6% (n=33) of the patients. The majority of hospitalizations were for observation (90.9%, n=30).
Discussion: Based on our preliminary data, ESD is safe and effective for resection of distal rectal lesions within 2 cm of the dentate line with a high rate of en bloc and R0 resection. Additional data from other centers is pending which will validate our findings. ESD may offer an excellent option for distal rectal lesions where transanal resection from colorectal surgery has technical limitations.

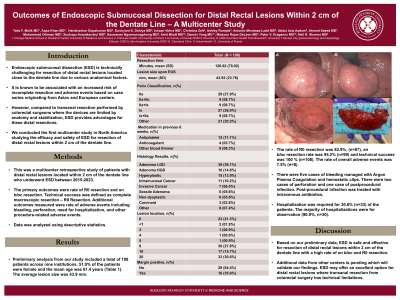
Figure: Figure 1. Endoscopic submucosal dissection for distal rectal lesion within 2 cm of the dentate line. Pre-resection (A), Pre-resection-Retroflexed view (B), Post-resection scar bed (C), Resected lesion (D).
Disclosures:
Talia Malik indicated no relevant financial relationships.
Aqsa Khan indicated no relevant financial relationships.
Harishankar Gopakumar indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Ishaan Vohra indicated no relevant financial relationships.
Christina Zelt indicated no relevant financial relationships.
Ashley Rumple indicated no relevant financial relationships.
Antonio Mendoza-Ladd indicated no relevant financial relationships.
Abdul Aadam indicated no relevant financial relationships.
Ahmed Saeed indicated no relevant financial relationships.
Mohamed Othman: AbbVie Inc. – Consultant, Grant/Research Support. Apollo – Consultant. Boston Scientific Coporation – Consultant, Grant/Research Support. ConMed – Consultant, Grant/Research Support. Creo Medical – Consultant. Lucid Diagnostics – Grant/Research Support. Lumendi – Consultant. Olympus – Consultant.
Suchapa Arayakarnkul indicated no relevant financial relationships.
Saowanee Ngamruengphong indicated no relevant financial relationships.
Amit Bhatt: Boston Scientific – Consultant. Medtronic – Consultant, Intellectual Property/Patents. Steris – Consultant.
Dennis Yang: 3D Matrix – Consultant, Grant/Research Support. Boston Scientific – Consultant. Fujifilm – Consultant. Medtronic – Consultant. Microtech – Consultant, Grant/Research Support. Neptune Medical – Consultant. Olympus – Consultant.
Mariajose Rojas DeLeon: Boston Scientific – Consultant.
Peter Draganov indicated no relevant financial relationships.
Neil Sharma indicated no relevant financial relationships.
Talia F.. Malik, MD1, Aqsa Khan, MD2, Harishankar Gopakumar, MD3, Dushyant Singh. Dahiya, MD4, Ishaan Vohra, MD3, Christina Zelt, BSN, RN2, Ashley Rumple, RN, BSN2, Antonio Mendoza-Ladd, MD5, Abdul Aziz. Aadam, MD6, Ahmed Saeed, MD7, Mohamed O. Othman, MD8, Suchapa Arayakarnkul, MD9, Saowanee Ngamruengphong, MD10, Amit Bhatt, MD11, Dennis Yang, MD12, Mariajose Rojas DeLeon, MD2, Peter V.. Draganov, MD13, Neil R.. Sharma, MD14. P3698 - Outcomes of Endoscopic Submucosal Dissection for Distal Rectal Lesions Within 2 Cm of the Dentate Line – A Multicenter Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
