Tuesday Poster Session
Category: Interventional Endoscopy
P3703 - Outcomes of Endoscopic Retrograde Cholangiopancreatography in Patients With Non-Alcoholic Steatohepatitis: A Nationwide Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AD
Ameya Deshmukh, DO
Saint Louis University
St. Louis, MO
Presenting Author(s)
Ameya deshmukh, DO1, Parth Desai, DO2, Hayden Rotramel, MD1, Abdallah El Alayli, MD1, Eugene Nwankwo, MD3, Timothy Chrusciel, MPH4, Michelle Baliss, DO1, Pradeep Yarra, MD1, Manavi Bhagwat, MD5, Antonio Cheesman, MD3
1Saint Louis University, St. Louis, MO; 2Tower Health-Reading Hospital, Reading, PA; 3Saint Louis University Hospital, St. Louis, MO; 4Advanced Health Data Research Institute (AHEAD), St. Louis, MO; 5Rush University Medical Center, Chicago, IL
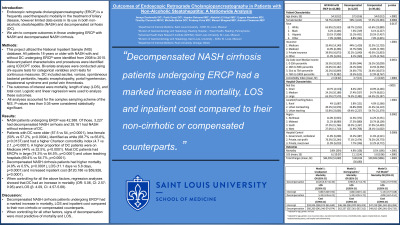
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a frequently used therapeutic modality in the treatment of biliary disease, however limited data exists in its use in both non-alcoholic steatohepatitis (NASH) and decompensated cirrhosis (DC). We aim to compare outcomes in those undergoing ERCP with NASH and decompensated NASH cirrhosis.
Methods: This project utilized the National Inpatient Sample (NIS) database. All patients 18 years or older with NASH with and without DC undergoing ERCP were identified from 2008 to 2015. Relevant patient characteristics and procedures were identified using ICD/CPT codes. Bivariate analyses were conducted using chi-square tests for categorical variables and t-tests for continuous measures. DC included ascites, varices, spontaneous bacterial peritonitis, hepatic encephalopathy, portal hypertension, hepatorenal syndrome and portal vein thrombosis. The outcomes of interest were mortality, length of stay (LOS), and total cost. Logistic and linear regression were used to analyze these outcomes. All analyses accounted for the complex sampling scheme of the NIS. P-values less than 0.05 were considered statistically significant.
Results: The total number of NASH patients undergoing ERCP was 42,388. Of those, 3,227 had decompensated NASH cirrhosis and 39,161 had NASH without evidence of DC. Patients with DC were older (57.5 vs 54, p< 0.0001), less female (50% vs 57.2%, p=0.0004), identified as white (68.7% vs 65.6%, p=0.0137) and had a higher Charlson comorbidity index (4.7 vs 2.1, p< 0.0001). A higher proportion of DC patients were on Medicare (44% vs 32.5%, p< 0.0001). Most DC patients had ERCPs in large (74.3% vs 64.5%, p< 0.0001) and urban teaching hospitals (69.4% vs 54.7%, p< 0.0001). Decompensated NASH cirrhosis patients had higher mortality (4.9% vs 0.5%, p< 0.0001), LOS (11.1 days vs 5.8 days, p< 0.0001) and increased inpatient cost ($120,186 vs $59,926, p< 0.0001). When controlling for all the above factors, regression analyses showed that DC had an increase in mortality (OR: 5.06, CI: 2.57-9.95) and LOS (β: 4.09, CI: 4.57-5.68).
Discussion: Decompensated NASH cirrhosis patients undergoing ERCP had a marked increase in mortality, LOS and inpatient cost compared to their non-cirrhotic or compensated counterparts. When controlling for all other factors, signs of decompensation were most predictive of mortality and LOS.
Disclosures:
Ameya deshmukh, DO1, Parth Desai, DO2, Hayden Rotramel, MD1, Abdallah El Alayli, MD1, Eugene Nwankwo, MD3, Timothy Chrusciel, MPH4, Michelle Baliss, DO1, Pradeep Yarra, MD1, Manavi Bhagwat, MD5, Antonio Cheesman, MD3. P3703 - Outcomes of Endoscopic Retrograde Cholangiopancreatography in Patients With Non-Alcoholic Steatohepatitis: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Louis University, St. Louis, MO; 2Tower Health-Reading Hospital, Reading, PA; 3Saint Louis University Hospital, St. Louis, MO; 4Advanced Health Data Research Institute (AHEAD), St. Louis, MO; 5Rush University Medical Center, Chicago, IL
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a frequently used therapeutic modality in the treatment of biliary disease, however limited data exists in its use in both non-alcoholic steatohepatitis (NASH) and decompensated cirrhosis (DC). We aim to compare outcomes in those undergoing ERCP with NASH and decompensated NASH cirrhosis.
Methods: This project utilized the National Inpatient Sample (NIS) database. All patients 18 years or older with NASH with and without DC undergoing ERCP were identified from 2008 to 2015. Relevant patient characteristics and procedures were identified using ICD/CPT codes. Bivariate analyses were conducted using chi-square tests for categorical variables and t-tests for continuous measures. DC included ascites, varices, spontaneous bacterial peritonitis, hepatic encephalopathy, portal hypertension, hepatorenal syndrome and portal vein thrombosis. The outcomes of interest were mortality, length of stay (LOS), and total cost. Logistic and linear regression were used to analyze these outcomes. All analyses accounted for the complex sampling scheme of the NIS. P-values less than 0.05 were considered statistically significant.
Results: The total number of NASH patients undergoing ERCP was 42,388. Of those, 3,227 had decompensated NASH cirrhosis and 39,161 had NASH without evidence of DC. Patients with DC were older (57.5 vs 54, p< 0.0001), less female (50% vs 57.2%, p=0.0004), identified as white (68.7% vs 65.6%, p=0.0137) and had a higher Charlson comorbidity index (4.7 vs 2.1, p< 0.0001). A higher proportion of DC patients were on Medicare (44% vs 32.5%, p< 0.0001). Most DC patients had ERCPs in large (74.3% vs 64.5%, p< 0.0001) and urban teaching hospitals (69.4% vs 54.7%, p< 0.0001). Decompensated NASH cirrhosis patients had higher mortality (4.9% vs 0.5%, p< 0.0001), LOS (11.1 days vs 5.8 days, p< 0.0001) and increased inpatient cost ($120,186 vs $59,926, p< 0.0001). When controlling for all the above factors, regression analyses showed that DC had an increase in mortality (OR: 5.06, CI: 2.57-9.95) and LOS (β: 4.09, CI: 4.57-5.68).
Discussion: Decompensated NASH cirrhosis patients undergoing ERCP had a marked increase in mortality, LOS and inpatient cost compared to their non-cirrhotic or compensated counterparts. When controlling for all other factors, signs of decompensation were most predictive of mortality and LOS.
Disclosures:
Ameya deshmukh indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Abdallah El Alayli indicated no relevant financial relationships.
Eugene Nwankwo indicated no relevant financial relationships.
Timothy Chrusciel indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Manavi Bhagwat indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Ameya deshmukh, DO1, Parth Desai, DO2, Hayden Rotramel, MD1, Abdallah El Alayli, MD1, Eugene Nwankwo, MD3, Timothy Chrusciel, MPH4, Michelle Baliss, DO1, Pradeep Yarra, MD1, Manavi Bhagwat, MD5, Antonio Cheesman, MD3. P3703 - Outcomes of Endoscopic Retrograde Cholangiopancreatography in Patients With Non-Alcoholic Steatohepatitis: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
