Tuesday Poster Session
Category: Interventional Endoscopy
P3704 - Trends in Indications and Outcomes for Endoscopic Retrograde Cholangiopancreatography in Non-Alcoholic Steatohepatitis Patients
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AD
Ameya Deshmukh, DO
Saint Louis University
St. Louis, MO
Presenting Author(s)
Ameya deshmukh, DO1, Parth Desai, DO2, Timothy Chrusciel, MPH3, Hayden Rotramel, MD1, Ryan Plunkett, MD1, Eugene Nwankwo, MD4, Rohan Tripathi, BS1, Neel Matiwala, BS1, Michelle Baliss, DO1, Antonio Cheesman, MD4
1Saint Louis University, St. Louis, MO; 2Tower Health-Reading Hospital, Reading, PA; 3Advanced Health Data Research Institute (AHEAD), St. Louis, MO; 4Saint Louis University Hospital, St. Louis, MO
Introduction: Non-alcoholic steatohepatitis (NASH) is on the rise within both the United States and global populations. Prior studies have shown NAFLD and NASH patients may be at a higher risk of post-endoscopic retrograde cholangiopancreatography (ERCP) adverse events such as post-ERCP pancreatitis. We seek to evaluate the trends for indications and outcomes for those within this patient population undergoing ERCP.
Methods: This project used the National Inpatient Sample (NIS) database. All patients 18 years or older with NASH undergoing ERCP were identified from 2008 to 2015. Relevant patient characteristics and procedures were identified using ICD/CPT codes. Linear regression was used for trend analysis. ERCP indications included acute pancreatitis, cholangitis, cholecystitis, choledocholithiasis and pancreatic mass. The outcomes of interest were pancreatitis, cholecystitis, infection, perforation, gastrointestinal (GI) bleeding, length of stay (LOS), and total inpatient cost. All analyses accounted for the complex sampling scheme of the NIS. P-values less than 0.05 were considered statistically significant.
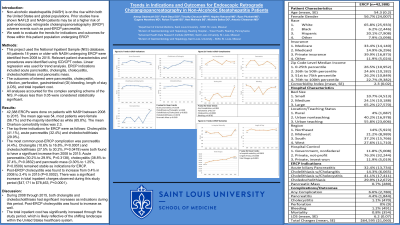
Results: A total of 42,388 ERCPs were done on patients with NASH between 2008 to 2015. The mean age was 54, most patients were female (56.7%) and the majority identified as white (65.8%). The mean Charlson comorbidity index was 2.3. The top three indications for ERCP were as follows: Cholecystitis (41.1%), acute pancreatitis (32.4%) and choledocholithiasis (29.9%). The most common post-ERCP complication was pancreatitis (4.4%). Cholangitis (10.6% to 16.8%, P< 0.0001) and choledocholithiasis (27.5% to 30.2%, P=0.0478) were both found to have a statistically significant increase from 2008 to 2015. Acute pancreatitis (30.2% to 29.9%, P=0.3138), cholecystitis (38.8% to 37.4%, P=0.0832) and pancreatic mass (0.30% to 1.25%, P=0.0509) remained stable as indications for ERCP through this time period. Post-ERCP cholecystitis was found to increase from 0.4% in 2008 to 2.4% in 2015 (P=0.0002). There was a significant increase in total inpatient charges observed during this study period ($47,171 to $78,463, P< 0.0001).
Discussion: During 2008 through 2015, both cholangitis and choledocholithiasis had significant increases as indications during this period. Additionally, post-ERCP cholecystitis was found to increase as well. The total inpatient cost has significantly increased through the study period, which is likely reflective of the shifting landscape within the United States healthcare system.

Disclosures:
Ameya deshmukh, DO1, Parth Desai, DO2, Timothy Chrusciel, MPH3, Hayden Rotramel, MD1, Ryan Plunkett, MD1, Eugene Nwankwo, MD4, Rohan Tripathi, BS1, Neel Matiwala, BS1, Michelle Baliss, DO1, Antonio Cheesman, MD4. P3704 - Trends in Indications and Outcomes for Endoscopic Retrograde Cholangiopancreatography in Non-Alcoholic Steatohepatitis Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Louis University, St. Louis, MO; 2Tower Health-Reading Hospital, Reading, PA; 3Advanced Health Data Research Institute (AHEAD), St. Louis, MO; 4Saint Louis University Hospital, St. Louis, MO
Introduction: Non-alcoholic steatohepatitis (NASH) is on the rise within both the United States and global populations. Prior studies have shown NAFLD and NASH patients may be at a higher risk of post-endoscopic retrograde cholangiopancreatography (ERCP) adverse events such as post-ERCP pancreatitis. We seek to evaluate the trends for indications and outcomes for those within this patient population undergoing ERCP.
Methods: This project used the National Inpatient Sample (NIS) database. All patients 18 years or older with NASH undergoing ERCP were identified from 2008 to 2015. Relevant patient characteristics and procedures were identified using ICD/CPT codes. Linear regression was used for trend analysis. ERCP indications included acute pancreatitis, cholangitis, cholecystitis, choledocholithiasis and pancreatic mass. The outcomes of interest were pancreatitis, cholecystitis, infection, perforation, gastrointestinal (GI) bleeding, length of stay (LOS), and total inpatient cost. All analyses accounted for the complex sampling scheme of the NIS. P-values less than 0.05 were considered statistically significant.
Results: A total of 42,388 ERCPs were done on patients with NASH between 2008 to 2015. The mean age was 54, most patients were female (56.7%) and the majority identified as white (65.8%). The mean Charlson comorbidity index was 2.3. The top three indications for ERCP were as follows: Cholecystitis (41.1%), acute pancreatitis (32.4%) and choledocholithiasis (29.9%). The most common post-ERCP complication was pancreatitis (4.4%). Cholangitis (10.6% to 16.8%, P< 0.0001) and choledocholithiasis (27.5% to 30.2%, P=0.0478) were both found to have a statistically significant increase from 2008 to 2015. Acute pancreatitis (30.2% to 29.9%, P=0.3138), cholecystitis (38.8% to 37.4%, P=0.0832) and pancreatic mass (0.30% to 1.25%, P=0.0509) remained stable as indications for ERCP through this time period. Post-ERCP cholecystitis was found to increase from 0.4% in 2008 to 2.4% in 2015 (P=0.0002). There was a significant increase in total inpatient charges observed during this study period ($47,171 to $78,463, P< 0.0001).
Discussion: During 2008 through 2015, both cholangitis and choledocholithiasis had significant increases as indications during this period. Additionally, post-ERCP cholecystitis was found to increase as well. The total inpatient cost has significantly increased through the study period, which is likely reflective of the shifting landscape within the United States healthcare system.

Figure: Figure 1: Trends in ERCP indications (A). Trends in ERCP complications (B). Trends in ERCP outcomes (C).
Disclosures:
Ameya deshmukh indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Timothy Chrusciel indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Ryan Plunkett indicated no relevant financial relationships.
Eugene Nwankwo indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Neel Matiwala indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Ameya deshmukh, DO1, Parth Desai, DO2, Timothy Chrusciel, MPH3, Hayden Rotramel, MD1, Ryan Plunkett, MD1, Eugene Nwankwo, MD4, Rohan Tripathi, BS1, Neel Matiwala, BS1, Michelle Baliss, DO1, Antonio Cheesman, MD4. P3704 - Trends in Indications and Outcomes for Endoscopic Retrograde Cholangiopancreatography in Non-Alcoholic Steatohepatitis Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
