Tuesday Poster Session
Category: Interventional Endoscopy
P3710 - The Efficacy and Safety of EUS-Guided Portal Pressure Gradient with Concomitant EUS-Guided Liver Biopsy in Patients with Chronic Liver Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Muhammad Nadeem Nadeem Yousaf, MD
University of Missouri-Columbia
Columbia, MO
Presenting Author(s)
Muhammad Nadeem. Yousaf, MD1, Nicholas McGhee, MD2, Jacob W. Cebulko, BS3, Darian Fard, MD2, Xheni Deda, MD2, Sanket Basida, MD1, Ahmed I.A. Swi, MD1, Niraj Shah, MD1, Ahmad Ali, MD4, Jamal A. Ibdah, MD2, Ghassan M. Hammoud, MD1
1University of Missouri-Columbia, Columbia, MO; 2University of Missouri, Columbia, MO; 3University of Missouri School of Medicine, Columbia, MO; 4Missouri University Hospital, Columbia, MO
Introduction: Liver elastography (LE), and Portal pressure gradient measurement (PPGM) are essential tools to predict prognosis and to guide for the management of patients with chronic liver disease. There is lack of data to establish cutoff values of EUS-guided liver stiffness by Shear Wave Measurement (SWM) that correlates with stage of liver fibrosis. We aimed to determine the efficacy and safety of EUS-PPGM and correlation of EUS-LE, EUS-PPGM values with stages of liver fibrosis in patients who underwent concomitant EUS-guided liver biopsy (EUS-LB).
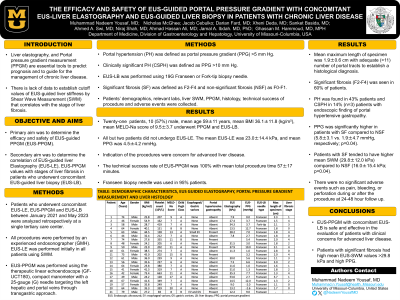
Methods: Patients who underwent concomitant EUS-LE, EUS-PPGM and EUS-LB between January 2021 and May 2023 were analyzed retrospectively at a single tertiary care center. EUS-LE was performed initially in all patients using SWM. EUS-PPGM was performed using therapeutic linear echoendoscope, compact manometer with a 25-gauge (G) needle targeting the left hepatic and portal veins through transgastric approach. Portal hypertension (PH) is defined as portal pressure gradient (PPG) >5 mmHg and clinically significant PH (CSPH) >10 mmHg. EUS-LB was performed using 19G Franseen or Fork-tip biopsy needle. Significant fibrosis (SF) was defined as F2-F4 and non-significant fibrosis (NSF) as F0-F1.
Results: Twenty-one patients, 57% (n=12) male, mean age 59±11 years, mean BMI 36.1±11.8 (kg/m
2
), mean MELD-Na score of 9.5±3.7 underwent PPGM and EUS-LB. All but two patients did not undergo EUS-LE. Indications of the procedures were clinical concern for advanced liver disease. The technical success rate of EUS-PPGM was 100% with mean total procedure time 57±17 minutes. Franseen biopsy needle was used in 95% of patients. Mean maximum length of specimen was 1.9±0.6 cm with adequate ( >11) number of portal tracts to establish a histological diagnosis. SF was seen in 60% of patients. The mean EUS-LE by SWM was 23.0±14.4 kPa, and mean PPG was 4.5±4.2 mmHg. PH was found in 43% patients and CSPH in 14% (n=3) patients. PPG was significantly higher in patients with SF compared to NSF (5.8±3.1 vs. 1.9±4.7 mmHg, respectively; p=0.04). Patients with SF have higher mean SWM (29.8±12.0 kPa) compared to NSF (16.0±15.4 kPa; p=0.04). There were no significant adverse events such as pain, bleeding, or perforation during or after the procedure at 24-48 hour follow up.
Discussion: EUS-PPGM with concomitant EUS-LB is safe and effective in the evaluation of patients with clinical concerns for advanced liver disease. Patients with significant fibrosis had high mean EUS-SWM values >29.8 kPa.
Disclosures:
Muhammad Nadeem. Yousaf, MD1, Nicholas McGhee, MD2, Jacob W. Cebulko, BS3, Darian Fard, MD2, Xheni Deda, MD2, Sanket Basida, MD1, Ahmed I.A. Swi, MD1, Niraj Shah, MD1, Ahmad Ali, MD4, Jamal A. Ibdah, MD2, Ghassan M. Hammoud, MD1. P3710 - The Efficacy and Safety of EUS-Guided Portal Pressure Gradient with Concomitant EUS-Guided Liver Biopsy in Patients with Chronic Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Columbia, Columbia, MO; 2University of Missouri, Columbia, MO; 3University of Missouri School of Medicine, Columbia, MO; 4Missouri University Hospital, Columbia, MO
Introduction: Liver elastography (LE), and Portal pressure gradient measurement (PPGM) are essential tools to predict prognosis and to guide for the management of patients with chronic liver disease. There is lack of data to establish cutoff values of EUS-guided liver stiffness by Shear Wave Measurement (SWM) that correlates with stage of liver fibrosis. We aimed to determine the efficacy and safety of EUS-PPGM and correlation of EUS-LE, EUS-PPGM values with stages of liver fibrosis in patients who underwent concomitant EUS-guided liver biopsy (EUS-LB).
Methods: Patients who underwent concomitant EUS-LE, EUS-PPGM and EUS-LB between January 2021 and May 2023 were analyzed retrospectively at a single tertiary care center. EUS-LE was performed initially in all patients using SWM. EUS-PPGM was performed using therapeutic linear echoendoscope, compact manometer with a 25-gauge (G) needle targeting the left hepatic and portal veins through transgastric approach. Portal hypertension (PH) is defined as portal pressure gradient (PPG) >5 mmHg and clinically significant PH (CSPH) >10 mmHg. EUS-LB was performed using 19G Franseen or Fork-tip biopsy needle. Significant fibrosis (SF) was defined as F2-F4 and non-significant fibrosis (NSF) as F0-F1.
Results: Twenty-one patients, 57% (n=12) male, mean age 59±11 years, mean BMI 36.1±11.8 (kg/m
2
), mean MELD-Na score of 9.5±3.7 underwent PPGM and EUS-LB. All but two patients did not undergo EUS-LE. Indications of the procedures were clinical concern for advanced liver disease. The technical success rate of EUS-PPGM was 100% with mean total procedure time 57±17 minutes. Franseen biopsy needle was used in 95% of patients. Mean maximum length of specimen was 1.9±0.6 cm with adequate ( >11) number of portal tracts to establish a histological diagnosis. SF was seen in 60% of patients. The mean EUS-LE by SWM was 23.0±14.4 kPa, and mean PPG was 4.5±4.2 mmHg. PH was found in 43% patients and CSPH in 14% (n=3) patients. PPG was significantly higher in patients with SF compared to NSF (5.8±3.1 vs. 1.9±4.7 mmHg, respectively; p=0.04). Patients with SF have higher mean SWM (29.8±12.0 kPa) compared to NSF (16.0±15.4 kPa; p=0.04). There were no significant adverse events such as pain, bleeding, or perforation during or after the procedure at 24-48 hour follow up.
Discussion: EUS-PPGM with concomitant EUS-LB is safe and effective in the evaluation of patients with clinical concerns for advanced liver disease. Patients with significant fibrosis had high mean EUS-SWM values >29.8 kPa.
Disclosures:
Muhammad Yousaf indicated no relevant financial relationships.
Nicholas McGhee indicated no relevant financial relationships.
Jacob Cebulko indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Xheni Deda indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Ahmed Swi indicated no relevant financial relationships.
Niraj Shah indicated no relevant financial relationships.
Ahmad Ali indicated no relevant financial relationships.
Jamal Ibdah indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Muhammad Nadeem. Yousaf, MD1, Nicholas McGhee, MD2, Jacob W. Cebulko, BS3, Darian Fard, MD2, Xheni Deda, MD2, Sanket Basida, MD1, Ahmed I.A. Swi, MD1, Niraj Shah, MD1, Ahmad Ali, MD4, Jamal A. Ibdah, MD2, Ghassan M. Hammoud, MD1. P3710 - The Efficacy and Safety of EUS-Guided Portal Pressure Gradient with Concomitant EUS-Guided Liver Biopsy in Patients with Chronic Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
