Tuesday Poster Session
Category: Interventional Endoscopy
P3715 - Success Rates of Fixation Techniques on Esophageal Stent Migration: A Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Daryl Ramai, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Daryl Ramai, MD, MSc1, Apostolis Papaefthymiou, MD, PhD2, Paraskevas Gkolfakis, MD3, Kirill Basiliya, MD2, Georgios Tziatzios, MD3, Vinay Sehgal, MD2, Andrea Telese, MD2, Benjamin Norton, MD2, Nasar Aslam, MD2, Gavin Johnson, MD2, Rehan Haidry, MD2
1University of Utah, Salt Lake City, UT; 2University College London Hospitals, London, England, United Kingdom; 3General Hospital of Nea Ionia, Athens, Attiki, Greece
Introduction: Esophageal stenting (ES) for benign and malignant diseases of the esophagus are an important intervention for the management of dysphagia. Stent migration represents a common drawback for this procedure. This systematic review with meta-analysis aimed to assess the benefit of ES fixation over non-fixated stenting.
Methods: : A systematic research was performed in MEDLINE, Cochrane, Scopus and ClinicalTrials.gov databases until January 2023 for comparative studies evaluating the migration rates of ES after anchoring or not. Quality assessment was based on the Newcastle-Ottawa Scale. The primary outcome included the relative difference of migration rates for fixated and non-fixated ES, with the rate of adverse events being the secondary outcome. A subgroup analysis was conducted to stratify the results based on different fixation techniques; suturing, over the scope clipping (OTSC) and trough the scope clipping (TTSC). We performed meta-analyses using a random effects model and the results were reported as odds ratios (OR), with 95% Confidence Intervals (95%CI).
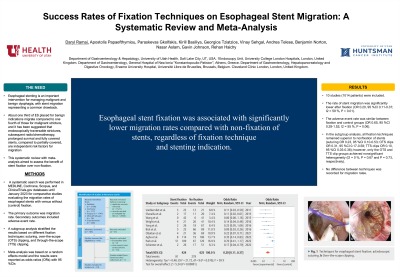
Results: Ten studies (1014 patients) were included to our analysis. The rates of self-expandable metal stent (SEMS) migration were significantly lower after fixation with an OR=0.20 (95%CI: 0.11-0.37; I2=59%). With regard to the secondary outcome, the rates of adverse events were similar between the fixation and control groups [OR=0.65 (95%CI: 0.28-1.52; I2=55%)], and no death related to the procedure was recorded. In the subgroup analysis, all anchoring techniques preserved the superiority over non-fixated stents [suturing OR= 0.23 (95%CI: 0.10-0.53); OTSC OR= 0.31 (95%CI: 0.17- 0.58); TTSC OR=0.10 (95%CI: 0.03-0.38)], however only OTSC and TTSC groups achieved non-significant heterogeneity (I2=0%). No difference between techniques was recorded considering the migration rates.
Discussion: Esophageal stent fixation is associated with significantly lower migration and low complication rates compared to the non-fixated SEMS regardless its type and stenting indication.

Disclosures:
Daryl Ramai, MD, MSc1, Apostolis Papaefthymiou, MD, PhD2, Paraskevas Gkolfakis, MD3, Kirill Basiliya, MD2, Georgios Tziatzios, MD3, Vinay Sehgal, MD2, Andrea Telese, MD2, Benjamin Norton, MD2, Nasar Aslam, MD2, Gavin Johnson, MD2, Rehan Haidry, MD2. P3715 - Success Rates of Fixation Techniques on Esophageal Stent Migration: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2University College London Hospitals, London, England, United Kingdom; 3General Hospital of Nea Ionia, Athens, Attiki, Greece
Introduction: Esophageal stenting (ES) for benign and malignant diseases of the esophagus are an important intervention for the management of dysphagia. Stent migration represents a common drawback for this procedure. This systematic review with meta-analysis aimed to assess the benefit of ES fixation over non-fixated stenting.
Methods: : A systematic research was performed in MEDLINE, Cochrane, Scopus and ClinicalTrials.gov databases until January 2023 for comparative studies evaluating the migration rates of ES after anchoring or not. Quality assessment was based on the Newcastle-Ottawa Scale. The primary outcome included the relative difference of migration rates for fixated and non-fixated ES, with the rate of adverse events being the secondary outcome. A subgroup analysis was conducted to stratify the results based on different fixation techniques; suturing, over the scope clipping (OTSC) and trough the scope clipping (TTSC). We performed meta-analyses using a random effects model and the results were reported as odds ratios (OR), with 95% Confidence Intervals (95%CI).
Results: Ten studies (1014 patients) were included to our analysis. The rates of self-expandable metal stent (SEMS) migration were significantly lower after fixation with an OR=0.20 (95%CI: 0.11-0.37; I2=59%). With regard to the secondary outcome, the rates of adverse events were similar between the fixation and control groups [OR=0.65 (95%CI: 0.28-1.52; I2=55%)], and no death related to the procedure was recorded. In the subgroup analysis, all anchoring techniques preserved the superiority over non-fixated stents [suturing OR= 0.23 (95%CI: 0.10-0.53); OTSC OR= 0.31 (95%CI: 0.17- 0.58); TTSC OR=0.10 (95%CI: 0.03-0.38)], however only OTSC and TTSC groups achieved non-significant heterogeneity (I2=0%). No difference between techniques was recorded considering the migration rates.
Discussion: Esophageal stent fixation is associated with significantly lower migration and low complication rates compared to the non-fixated SEMS regardless its type and stenting indication.

Figure: Forest plot reporting the odds ratios of migration rates between fixated and non-fixated esophageal stents
Disclosures:
Daryl Ramai indicated no relevant financial relationships.
Apostolis Papaefthymiou indicated no relevant financial relationships.
Paraskevas Gkolfakis indicated no relevant financial relationships.
Kirill Basiliya indicated no relevant financial relationships.
Georgios Tziatzios indicated no relevant financial relationships.
Vinay Sehgal indicated no relevant financial relationships.
Andrea Telese indicated no relevant financial relationships.
Benjamin Norton indicated no relevant financial relationships.
Nasar Aslam indicated no relevant financial relationships.
Gavin Johnson indicated no relevant financial relationships.
Rehan Haidry indicated no relevant financial relationships.
Daryl Ramai, MD, MSc1, Apostolis Papaefthymiou, MD, PhD2, Paraskevas Gkolfakis, MD3, Kirill Basiliya, MD2, Georgios Tziatzios, MD3, Vinay Sehgal, MD2, Andrea Telese, MD2, Benjamin Norton, MD2, Nasar Aslam, MD2, Gavin Johnson, MD2, Rehan Haidry, MD2. P3715 - Success Rates of Fixation Techniques on Esophageal Stent Migration: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
