Tuesday Poster Session
Category: Interventional Endoscopy
P3716 - EUS-Guided Biliary Drainage vs ERCP Drainage for Unresectable Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- SP
Spyros Peppas, MD
MedStar Health/Georgetown-Washington Hospital Center
Washington, DC
Presenting Author(s)
Spyros Peppas, MD1, Akram Ahmad, MBBS2, Nadera Altork, MD1, Sayel H. Alzraikat, MD1, Amer Arman, MD1, Won Kyoo Cho, MD3
1MedStar Health/Georgetown-Washington Hospital Center, Washington, DC; 2MedStar Georgetown Washington Hospital Center, Washington, DC; 3Inova Medical Group, Leesburg, VA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) with the insertion of self-expandable metal stents (SEMS) has been the preferred treatment modality for the palliation of malignant distal biliary obstruction (MDBO). Endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as an alternative primary option for relieving MDBO. Potential advantages include lower procedure-related pancreatitis, shorter procedure time and avoidance of placing the stent through the biliary stricture. This systematic review and meta-analysis aimed to compare the outcomes of EUS-BD versus ERCP on relieving MDBO.
Methods: We performed a literature search using the MEDLINE, Embase and Cochrane databases from inception until May 2023 to identify randomized controlled trials (RCTs) comparing the outcomes of EUS-BD and ERCP in patients with MDBO. The outcomes of interest included technical and clinical success, overall adverse events, procedure-related pancreatitis and post-procedural re-intervention. The quality of the studies was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB 2). Risk ratios (RRs) were calculated and pooled for each outcome. Meta-analysis was performed using the random effects model in STATA 17.0 software.
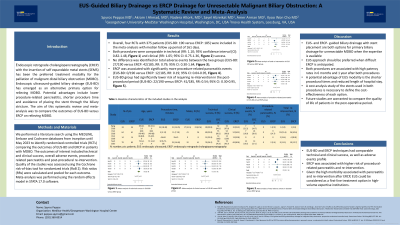
Results: Four RCTs with 375 patients (EUS-BD: 190 versus ERCP: 185) were included in the meta-analysis with a median follow-up period of 161 days. Both procedures were comparable in technical (RR: 1.10; 95% confidence interval [CI]: 0.82-1.48, Figure 1) and clinical (RR: 1.05; 95% CI: 0.75-1.36, Figure 2) success. No difference was identified on total adverse events between the two groups (EUS-BD: 27/190 versus ERCP: 42/185, RR: 0.79; 95% CI: 0.30-1.64, Figure 3); however, ERCP was associated with significantly more procedure-related pancreatitis events (EUS-BD: 0/190 versus ERCP: 12/185, RR: 0.19; 95% CI: 0.04-0.95, Figure 4). Additionally, the EUS-BD group had a significantly lower risk of requiring re-intervention in the post-procedural period (EUS-BD: 22/190 versus ERCP: 41/185, RR: 0.54; 95% CI: 0.30-0.95, Figure 5).
Discussion: Although, EUS-BD and ERCP techniques had comparable technical and clinical success, and adverse events profile, ERCP was associated with a higher risk of procedural-related pancreatitis and re-intervention. Given the high morbidity associated with pancreatitis and re-intervention after ERCP, EUS could be considered as a first-line treatment option in high-volume expertise institutions.

Disclosures:
Spyros Peppas, MD1, Akram Ahmad, MBBS2, Nadera Altork, MD1, Sayel H. Alzraikat, MD1, Amer Arman, MD1, Won Kyoo Cho, MD3. P3716 - EUS-Guided Biliary Drainage vs ERCP Drainage for Unresectable Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Health/Georgetown-Washington Hospital Center, Washington, DC; 2MedStar Georgetown Washington Hospital Center, Washington, DC; 3Inova Medical Group, Leesburg, VA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) with the insertion of self-expandable metal stents (SEMS) has been the preferred treatment modality for the palliation of malignant distal biliary obstruction (MDBO). Endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as an alternative primary option for relieving MDBO. Potential advantages include lower procedure-related pancreatitis, shorter procedure time and avoidance of placing the stent through the biliary stricture. This systematic review and meta-analysis aimed to compare the outcomes of EUS-BD versus ERCP on relieving MDBO.
Methods: We performed a literature search using the MEDLINE, Embase and Cochrane databases from inception until May 2023 to identify randomized controlled trials (RCTs) comparing the outcomes of EUS-BD and ERCP in patients with MDBO. The outcomes of interest included technical and clinical success, overall adverse events, procedure-related pancreatitis and post-procedural re-intervention. The quality of the studies was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB 2). Risk ratios (RRs) were calculated and pooled for each outcome. Meta-analysis was performed using the random effects model in STATA 17.0 software.
Results: Four RCTs with 375 patients (EUS-BD: 190 versus ERCP: 185) were included in the meta-analysis with a median follow-up period of 161 days. Both procedures were comparable in technical (RR: 1.10; 95% confidence interval [CI]: 0.82-1.48, Figure 1) and clinical (RR: 1.05; 95% CI: 0.75-1.36, Figure 2) success. No difference was identified on total adverse events between the two groups (EUS-BD: 27/190 versus ERCP: 42/185, RR: 0.79; 95% CI: 0.30-1.64, Figure 3); however, ERCP was associated with significantly more procedure-related pancreatitis events (EUS-BD: 0/190 versus ERCP: 12/185, RR: 0.19; 95% CI: 0.04-0.95, Figure 4). Additionally, the EUS-BD group had a significantly lower risk of requiring re-intervention in the post-procedural period (EUS-BD: 22/190 versus ERCP: 41/185, RR: 0.54; 95% CI: 0.30-0.95, Figure 5).
Discussion: Although, EUS-BD and ERCP techniques had comparable technical and clinical success, and adverse events profile, ERCP was associated with a higher risk of procedural-related pancreatitis and re-intervention. Given the high morbidity associated with pancreatitis and re-intervention after ERCP, EUS could be considered as a first-line treatment option in high-volume expertise institutions.

Figure: Forest plots of outcomes in EUS-BD versus ERCP group in patients with malignant biliary obstruction
Disclosures:
Spyros Peppas indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Nadera Altork indicated no relevant financial relationships.
Sayel Alzraikat indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Won Kyoo Cho indicated no relevant financial relationships.
Spyros Peppas, MD1, Akram Ahmad, MBBS2, Nadera Altork, MD1, Sayel H. Alzraikat, MD1, Amer Arman, MD1, Won Kyoo Cho, MD3. P3716 - EUS-Guided Biliary Drainage vs ERCP Drainage for Unresectable Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
