Tuesday Poster Session
Category: Interventional Endoscopy
P3752 - The Role of Laparoscopic-Assisted ERCP in Patients Following Roux-en-Y Gastric Bypass
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Lauren A. Lyssy, DO
St. David's South Austin Medical Center
Austin, TX
Presenting Author(s)
Lauren Lyssy, DO1, Jeremy Polman, DO, MS, MBA2
1St. David's South Austin Medical Center, Austin, TX; 2St. David's South Austin Medical Center, Nashville, TN
Introduction: Currently, over 40% of Americans are considered overweight or obese. This surge in obesity correlates with an increased number of bariatric surgeries, especially over the last decade. Some endoscopic procedures, such as ERCP (endoscopic retrograde cholangiopancreatography), may subsequently need to be modified to accommodate a patient’s post-operative anatomy. Here, we present a case of laparoscopic-assisted ERCP (LAERCP) performed for the treatment of choledocholithiasis in a patient with a history of bariatric surgery.
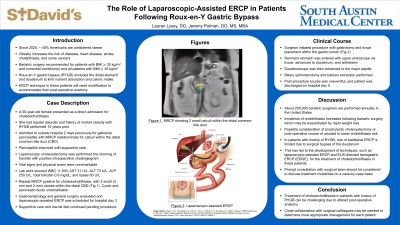
Case Description/Methods: A 50-year-old female with bipolar disorder and a history of morbid obesity with Roux-en-Y gastric bypass (RYGB) performed 10 years prior presented as a direct admission for choledocholithiasis. She was admitted to an outside hospital 2 days previously for epigastric pain and vomiting, receiving a diagnosis of gallstone pancreatitis. Her presenting symptoms resolved, and she underwent a laparoscopic cholecystectomy 1 day prior to transfer. An intraoperative cholangiogram was positive for filling defects in the distal common bile duct (CBD). She recovered well from surgery and was then transferred for consideration of a LAERCP. Upon transfer, vital signs were unremarkable. Lab work showed WBC 11,000, total bilirubin 0.6, AST 31, ALT 73, ALP 250, and lipase 60. Physical examination was remarkable for epigastric tenderness and intact laparoscopic incisions. An MRCP was positive for choledocholithiasis, with 2 small (2 and 3 mm) filling defects visualized in the distal CBD. On hospital day 3, a LAERCP was performed. A gastrotomy was created with a trocar placed within the gastric remnant, through which an upper endoscope was introduced and advanced to the duodenum. The upper endoscope was then removed and a duodenoscope was introduced. The remaining ERCP was accomplished without difficulty and multiple stones were removed. No stones remained as confirmed by cholangiogram. There were no complications and the patient recovered from the procedure well. She was discharged home on hospital day 5.
Discussion: In this patient, a traditional ERCP was unable to be performed due to her altered anatomy following a RYGB. Surgical consultation was necessary to perform a LAERCP to obtain access to the biliary tree. With approximately 200,000 bariatric surgeries performed annually in the United States, procedures such as LAERCP will likely become increasingly common, emphasizing the role of close interdisciplinary management in successful patient care.
Disclosures:
Lauren Lyssy, DO1, Jeremy Polman, DO, MS, MBA2. P3752 - The Role of Laparoscopic-Assisted ERCP in Patients Following Roux-en-Y Gastric Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. David's South Austin Medical Center, Austin, TX; 2St. David's South Austin Medical Center, Nashville, TN
Introduction: Currently, over 40% of Americans are considered overweight or obese. This surge in obesity correlates with an increased number of bariatric surgeries, especially over the last decade. Some endoscopic procedures, such as ERCP (endoscopic retrograde cholangiopancreatography), may subsequently need to be modified to accommodate a patient’s post-operative anatomy. Here, we present a case of laparoscopic-assisted ERCP (LAERCP) performed for the treatment of choledocholithiasis in a patient with a history of bariatric surgery.
Case Description/Methods: A 50-year-old female with bipolar disorder and a history of morbid obesity with Roux-en-Y gastric bypass (RYGB) performed 10 years prior presented as a direct admission for choledocholithiasis. She was admitted to an outside hospital 2 days previously for epigastric pain and vomiting, receiving a diagnosis of gallstone pancreatitis. Her presenting symptoms resolved, and she underwent a laparoscopic cholecystectomy 1 day prior to transfer. An intraoperative cholangiogram was positive for filling defects in the distal common bile duct (CBD). She recovered well from surgery and was then transferred for consideration of a LAERCP. Upon transfer, vital signs were unremarkable. Lab work showed WBC 11,000, total bilirubin 0.6, AST 31, ALT 73, ALP 250, and lipase 60. Physical examination was remarkable for epigastric tenderness and intact laparoscopic incisions. An MRCP was positive for choledocholithiasis, with 2 small (2 and 3 mm) filling defects visualized in the distal CBD. On hospital day 3, a LAERCP was performed. A gastrotomy was created with a trocar placed within the gastric remnant, through which an upper endoscope was introduced and advanced to the duodenum. The upper endoscope was then removed and a duodenoscope was introduced. The remaining ERCP was accomplished without difficulty and multiple stones were removed. No stones remained as confirmed by cholangiogram. There were no complications and the patient recovered from the procedure well. She was discharged home on hospital day 5.
Discussion: In this patient, a traditional ERCP was unable to be performed due to her altered anatomy following a RYGB. Surgical consultation was necessary to perform a LAERCP to obtain access to the biliary tree. With approximately 200,000 bariatric surgeries performed annually in the United States, procedures such as LAERCP will likely become increasingly common, emphasizing the role of close interdisciplinary management in successful patient care.
Disclosures:
Lauren Lyssy indicated no relevant financial relationships.
Jeremy Polman indicated no relevant financial relationships.
Lauren Lyssy, DO1, Jeremy Polman, DO, MS, MBA2. P3752 - The Role of Laparoscopic-Assisted ERCP in Patients Following Roux-en-Y Gastric Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
