Tuesday Poster Session
Category: Interventional Endoscopy
P3754 - Endoscopic Repair of Esophago-Respiratory Fistula With Amplatzer Device
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- BB
Benjamin E. Brier, MD
Naval Medical Center
San Diego, California
Presenting Author(s)
Benjamin E. Brier, MD1, Benjamin Fiore, MD1, Gordon Hunt, MD2
1Naval Medical Center, San Diego, CA; 2Kaiser Permanente, San Diego, CA
Introduction: Successful endoscopic repair of chronic esophago-respiratory fistula (ERF) was achieved using an Amplatzer septal occluder device (ASOD), in a patient who failed management with esophageal fully covered metal stent (EFCMS). This achieved clinical success despite suboptimal deployment.
Case Description/Methods: A 51-year-old woman with history of signet ring gastric adenocarcinoma underwent gastrectomy with enteric-esophageal anastomosis. She presented with recurrent pneumonias over three years and was found to have the formation of a chronic ERF. This persisted despite the placement of two separate EFCMS. She was considered a poor candidate for surgical repair so closure with ASOD was used.
Esophagastroduodenoscoy (EGD) demonstrated a 3 mm esophageal orifice of the ERF just proximal to the anastomosis. Carbon dioxide insufflation of the site caused an increase in the patient’s end tidal CO2 (from 30s to 170s mmHg) and physiologically confirmed its direct communication with the bronchial tree. The esophageal orifice of the fistula was treated with APC to promote granulation tissue. Then multiple attempts were made to seat a 6mm x 6 mm ASOD within the ERF, with distal flange in the bronchial tree and proximal in the esophagus. Size and angulation of the tract made this impossible. The device was then placed into the into the esophageal orifice and pediatric forceps were used to seat the device as deep into the fistula as possible. An endoclip was then used to approximate normal esophageal mucosa over the device and secure it in place.
Two months after placement of the ASOD, the patient had resolution of symptoms and no evidence of persistent ERF on esophagram.
Discussion: The standard endoscopic management of ERF is the use of EFMCS. When this management fails, alternative endoscopic treatments are limited. Other published cases have demonstrated the use of ASODs for this indication. However, these reports consistently demonstrate a more traditional placement of the device with flanges fully deployed on either side of the fistula. In our patient, it was difficult to optimally seat the ASOD due to small fistulous opening and angulation. Despite sub-optimal deployment, we still achieved clinical success. This highlights a novel use of the device, which may be more practical in technically challenging cases.

Disclosures:
Benjamin E. Brier, MD1, Benjamin Fiore, MD1, Gordon Hunt, MD2. P3754 - Endoscopic Repair of Esophago-Respiratory Fistula With Amplatzer Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Naval Medical Center, San Diego, CA; 2Kaiser Permanente, San Diego, CA
Introduction: Successful endoscopic repair of chronic esophago-respiratory fistula (ERF) was achieved using an Amplatzer septal occluder device (ASOD), in a patient who failed management with esophageal fully covered metal stent (EFCMS). This achieved clinical success despite suboptimal deployment.
Case Description/Methods: A 51-year-old woman with history of signet ring gastric adenocarcinoma underwent gastrectomy with enteric-esophageal anastomosis. She presented with recurrent pneumonias over three years and was found to have the formation of a chronic ERF. This persisted despite the placement of two separate EFCMS. She was considered a poor candidate for surgical repair so closure with ASOD was used.
Esophagastroduodenoscoy (EGD) demonstrated a 3 mm esophageal orifice of the ERF just proximal to the anastomosis. Carbon dioxide insufflation of the site caused an increase in the patient’s end tidal CO2 (from 30s to 170s mmHg) and physiologically confirmed its direct communication with the bronchial tree. The esophageal orifice of the fistula was treated with APC to promote granulation tissue. Then multiple attempts were made to seat a 6mm x 6 mm ASOD within the ERF, with distal flange in the bronchial tree and proximal in the esophagus. Size and angulation of the tract made this impossible. The device was then placed into the into the esophageal orifice and pediatric forceps were used to seat the device as deep into the fistula as possible. An endoclip was then used to approximate normal esophageal mucosa over the device and secure it in place.
Two months after placement of the ASOD, the patient had resolution of symptoms and no evidence of persistent ERF on esophagram.
Discussion: The standard endoscopic management of ERF is the use of EFMCS. When this management fails, alternative endoscopic treatments are limited. Other published cases have demonstrated the use of ASODs for this indication. However, these reports consistently demonstrate a more traditional placement of the device with flanges fully deployed on either side of the fistula. In our patient, it was difficult to optimally seat the ASOD due to small fistulous opening and angulation. Despite sub-optimal deployment, we still achieved clinical success. This highlights a novel use of the device, which may be more practical in technically challenging cases.

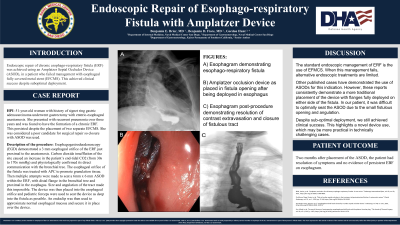
Figure: Esophagram demonstrating esophageal-respiratory fistula (Figure A). Amplatzer occlusion device as placed in fistula opening after being deployed in esophagus (Figure B). Esophagram post-procedure demonstrating resolution of contrast extravasation and closure of fistulous tract (Figure C).
Disclosures:
Benjamin Brier indicated no relevant financial relationships.
Benjamin Fiore indicated no relevant financial relationships.
Gordon Hunt indicated no relevant financial relationships.
Benjamin E. Brier, MD1, Benjamin Fiore, MD1, Gordon Hunt, MD2. P3754 - Endoscopic Repair of Esophago-Respiratory Fistula With Amplatzer Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
