Tuesday Poster Session
Category: Interventional Endoscopy
P3760 - Case Series: Application of Radiofrequency Ablation in Various Pancreatic Neoplastic Lesions
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Varshita Goduguchinta, DO
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Award: Presidential Poster Award
Varshita Goduguchinta, DO1, Ahamed Khalyfa, DO2, Navkiran Randhawa, DO3, Rahil Desai, DO4, Mahnoor Inamullah, MD5, Kamran Ayub, MD6
1Franciscan Health Olympia Fields, Chicago, IL; 2University of Iowa, Iowa City, IA; 3Augusta University, Medical College of Georgia, Dyer, IN; 4Franciscan Health Olympia Fields, Westlake, OH; 5Southwest Gastroenterology, a Division of GI Partners of Illinois, Oak Lawn, IL; 6Silver Cross Hospital, New Lenox, IL
Introduction: Treatment of pancreatic neoplasms is inherently dependent on clinical staging of disease and resectability of the tumor. However, surgical resection is not an option in some patients with comorbidities or other high risk features. Our aim was to study the efficacy and safety of endoscopic radiofrequency ablation (RFA) as an alternative to surgery as it was not an option in these patients. Our series includes patients with neuroendocrine tumors, adenocarcinoma and intraductal papillary mucinous neoplasm with malignant nodule.
Case Description/Methods: A 75-year-old male with a medical history of coronary artery disease, hypertension, hyperlipidemia, and iron deficiency anemia presented with abdominal pain. CT Abdomen/Pelvis was obtained and highlighted a subtle distal pancreatic mass. Endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNA) was later performed on the hypoechoic nodule measuring 15.6 x 12 mm in the pancreatic tail. Pathology identified the mass as a neuroendocrine tumor (NET). Surgery was felt to be extremely high-risk and the patient refused this option. An EUS-guided radiofrequency ablation (RFA) was performed using a 19-gauge RFA needle with 10 watts energy, with 6 applications (30, 21, 35, 22, 29, and 34 seconds). Follow up CT 8 weeks later demonstrated subtle disease at the pancreatic tail. Repeat EUS-FNA was performed and showed that the pancreatic mass had shrunk, now 11.3 mm x 7.2 mm. Repeat EUS-RFA was performed with 4 applications (15, 18, 23, and 26 seconds, respectively) using 10 watts energy. Follow up EUS 4 months later demonstrated the pancreatic NET had disappeared completely, now replaced by scar tissue. One year later, patient continues to do well without any signs of residual disease.
RFA was applied for 3 other patients with pancreatic neoplasias (NET, adenocarcinoma, and IPMN), with good to excellent response. Although NET had the best response to RFA, the other neoplasms responded well to RFA as demonstrated by reduction of initial tumor size (Table 1). One patient had pancreatitis and was hospitalized for 3 days, a second patient had abdominal pain for 2 days after the procedure. No other complications were encountered.
Discussion: With our case series, we show that EUS-RFA of pancreatic neoplasia is a viable option in selected patients who are not candidates for pancreatic surgery.

Disclosures:
Varshita Goduguchinta, DO1, Ahamed Khalyfa, DO2, Navkiran Randhawa, DO3, Rahil Desai, DO4, Mahnoor Inamullah, MD5, Kamran Ayub, MD6. P3760 - Case Series: Application of Radiofrequency Ablation in Various Pancreatic Neoplastic Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Varshita Goduguchinta, DO1, Ahamed Khalyfa, DO2, Navkiran Randhawa, DO3, Rahil Desai, DO4, Mahnoor Inamullah, MD5, Kamran Ayub, MD6
1Franciscan Health Olympia Fields, Chicago, IL; 2University of Iowa, Iowa City, IA; 3Augusta University, Medical College of Georgia, Dyer, IN; 4Franciscan Health Olympia Fields, Westlake, OH; 5Southwest Gastroenterology, a Division of GI Partners of Illinois, Oak Lawn, IL; 6Silver Cross Hospital, New Lenox, IL
Introduction: Treatment of pancreatic neoplasms is inherently dependent on clinical staging of disease and resectability of the tumor. However, surgical resection is not an option in some patients with comorbidities or other high risk features. Our aim was to study the efficacy and safety of endoscopic radiofrequency ablation (RFA) as an alternative to surgery as it was not an option in these patients. Our series includes patients with neuroendocrine tumors, adenocarcinoma and intraductal papillary mucinous neoplasm with malignant nodule.
Case Description/Methods: A 75-year-old male with a medical history of coronary artery disease, hypertension, hyperlipidemia, and iron deficiency anemia presented with abdominal pain. CT Abdomen/Pelvis was obtained and highlighted a subtle distal pancreatic mass. Endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNA) was later performed on the hypoechoic nodule measuring 15.6 x 12 mm in the pancreatic tail. Pathology identified the mass as a neuroendocrine tumor (NET). Surgery was felt to be extremely high-risk and the patient refused this option. An EUS-guided radiofrequency ablation (RFA) was performed using a 19-gauge RFA needle with 10 watts energy, with 6 applications (30, 21, 35, 22, 29, and 34 seconds). Follow up CT 8 weeks later demonstrated subtle disease at the pancreatic tail. Repeat EUS-FNA was performed and showed that the pancreatic mass had shrunk, now 11.3 mm x 7.2 mm. Repeat EUS-RFA was performed with 4 applications (15, 18, 23, and 26 seconds, respectively) using 10 watts energy. Follow up EUS 4 months later demonstrated the pancreatic NET had disappeared completely, now replaced by scar tissue. One year later, patient continues to do well without any signs of residual disease.
RFA was applied for 3 other patients with pancreatic neoplasias (NET, adenocarcinoma, and IPMN), with good to excellent response. Although NET had the best response to RFA, the other neoplasms responded well to RFA as demonstrated by reduction of initial tumor size (Table 1). One patient had pancreatitis and was hospitalized for 3 days, a second patient had abdominal pain for 2 days after the procedure. No other complications were encountered.
Discussion: With our case series, we show that EUS-RFA of pancreatic neoplasia is a viable option in selected patients who are not candidates for pancreatic surgery.

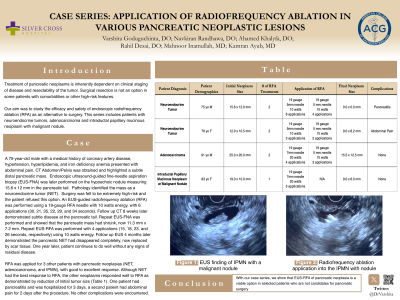
Figure: (Left) EUS finding of IPMN with malignant nodule; (Right) RFA application of the nodule
Disclosures:
Varshita Goduguchinta indicated no relevant financial relationships.
Ahamed Khalyfa indicated no relevant financial relationships.
Navkiran Randhawa indicated no relevant financial relationships.
Rahil Desai indicated no relevant financial relationships.
Mahnoor Inamullah indicated no relevant financial relationships.
Kamran Ayub indicated no relevant financial relationships.
Varshita Goduguchinta, DO1, Ahamed Khalyfa, DO2, Navkiran Randhawa, DO3, Rahil Desai, DO4, Mahnoor Inamullah, MD5, Kamran Ayub, MD6. P3760 - Case Series: Application of Radiofrequency Ablation in Various Pancreatic Neoplastic Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


