Tuesday Poster Session
Category: Interventional Endoscopy
P3763 - Post Operative Anastomotic Surgical Leakage Managed Conservatively with Endoscopic Vacuum Assisted Device
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MM
Mujtaba Mohamed, MBBS
Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Mohamed Hammad, MD1, Adnan Elghezewi, MD2, Mujtaba Mohamed, MBBS3, Ahmed Sherif, MD1, Wesam Frandah, MD2, M'hamed Turki, MD2
1Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Esophageal perforations are known complication of esophageal-gastric surgeries, stricture repair and bariatric surgery and it has mortality of 20%–50% and can be caused by iatrogenic factors, spontaneous events.The most alarming complication is an anastomotic leak, which raises death to 15% and total morbidity to 61%. Clinically presented with tachycardia, dyspnea, fever, chest and abdominal pain within several days post operation.EVAC among other endoscopic procedures are becoming more popular as an alternative for surgical intervention in management of perforation and anastomosis leakage
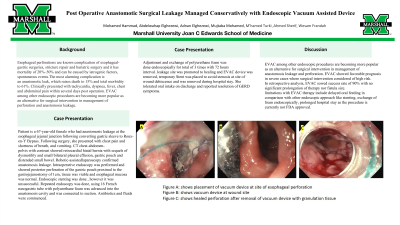
Case Description/Methods: Patient is a 67-year-old female who had anastomosis leakage at the esophageal jejunal junction following converting gastric sleeve to Roux-en-Y Bypass. Following surgery, she presented with chest pain and shortness of breath, and vomiting. CT chest-abdomen-pelvis with contrast showed retrocardial hiatal hernia with sequels of dysmotility and small bilateral pleural effusion, gastric pouch and distended small bowel. Robotic-assisted laparoscopy confirmed anastomosis leakage. Intraoperative endoscopy was performed and showed posterior perforation of the gastric pouch proximal to the gastrojejunostomy of 1cm, tissue was viable and esophageal mucosa was normal. Endoscopic stenting was done , however it was unsuccessful. Repeated endoscopy was done, using 16 French nasogastric tube with polyurethane foam was advanced into the anastomosis cavity and was connected to suction. Antibiotics and fluids were commenced. Adjustment and exchange of polyurethane foam was done endoscopically for total of 3 times with 72 hours interval. leakage site was promoted to healing and EVAC device was removed, temporary Stent was placed to avoid stenosis at site of wound dehiscence and was removed during hospital stay. She tolerated oral intake on discharge and reported resolution of GERD symptoms.
Discussion:
EVAC among other endoscopic procedures are becoming more popular as an alternative for surgical intervention in management of anastomosis leakage and perforation. EVAC showed favorable prognosis in severe cases where surgical intervention considered of high risk.
In retrospective analysis, EVAC sowed success rate of 90% with no significant prolongation of therapy nor fistula size.
limitations with EVAC therapy include delayed oral feeding in comparison with other endoscopic approach like stenting, exchange of foam endoscopically, prolonged hospital stay as the procedure is currently not FDA approved.

Disclosures:
Mohamed Hammad, MD1, Adnan Elghezewi, MD2, Mujtaba Mohamed, MBBS3, Ahmed Sherif, MD1, Wesam Frandah, MD2, M'hamed Turki, MD2. P3763 - Post Operative Anastomotic Surgical Leakage Managed Conservatively with Endoscopic Vacuum Assisted Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Esophageal perforations are known complication of esophageal-gastric surgeries, stricture repair and bariatric surgery and it has mortality of 20%–50% and can be caused by iatrogenic factors, spontaneous events.The most alarming complication is an anastomotic leak, which raises death to 15% and total morbidity to 61%. Clinically presented with tachycardia, dyspnea, fever, chest and abdominal pain within several days post operation.EVAC among other endoscopic procedures are becoming more popular as an alternative for surgical intervention in management of perforation and anastomosis leakage
Case Description/Methods: Patient is a 67-year-old female who had anastomosis leakage at the esophageal jejunal junction following converting gastric sleeve to Roux-en-Y Bypass. Following surgery, she presented with chest pain and shortness of breath, and vomiting. CT chest-abdomen-pelvis with contrast showed retrocardial hiatal hernia with sequels of dysmotility and small bilateral pleural effusion, gastric pouch and distended small bowel. Robotic-assisted laparoscopy confirmed anastomosis leakage. Intraoperative endoscopy was performed and showed posterior perforation of the gastric pouch proximal to the gastrojejunostomy of 1cm, tissue was viable and esophageal mucosa was normal. Endoscopic stenting was done , however it was unsuccessful. Repeated endoscopy was done, using 16 French nasogastric tube with polyurethane foam was advanced into the anastomosis cavity and was connected to suction. Antibiotics and fluids were commenced. Adjustment and exchange of polyurethane foam was done endoscopically for total of 3 times with 72 hours interval. leakage site was promoted to healing and EVAC device was removed, temporary Stent was placed to avoid stenosis at site of wound dehiscence and was removed during hospital stay. She tolerated oral intake on discharge and reported resolution of GERD symptoms.
Discussion:
EVAC among other endoscopic procedures are becoming more popular as an alternative for surgical intervention in management of anastomosis leakage and perforation. EVAC showed favorable prognosis in severe cases where surgical intervention considered of high risk.
In retrospective analysis, EVAC sowed success rate of 90% with no significant prolongation of therapy nor fistula size.
limitations with EVAC therapy include delayed oral feeding in comparison with other endoscopic approach like stenting, exchange of foam endoscopically, prolonged hospital stay as the procedure is currently not FDA approved.

Figure: Figure (A)(B)(C) shows use of EVAC in esophageal perforation
Disclosures:
Mohamed Hammad indicated no relevant financial relationships.
Adnan Elghezewi indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Endo gastric solutions – Consultant. Olympus Medical – Consultant.
M'hamed Turki indicated no relevant financial relationships.
Mohamed Hammad, MD1, Adnan Elghezewi, MD2, Mujtaba Mohamed, MBBS3, Ahmed Sherif, MD1, Wesam Frandah, MD2, M'hamed Turki, MD2. P3763 - Post Operative Anastomotic Surgical Leakage Managed Conservatively with Endoscopic Vacuum Assisted Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
