Tuesday Poster Session
Category: Interventional Endoscopy
P3764 - Endoscopic Closure of an Enterovaginal Fistula: Novel Use of a Cardiac Septal Occluder Device
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Scott Edelson, MD
Brooke Army Medical Center
San Antonio, Texas
Presenting Author(s)
Scott Edelson, MD, Cyrus Veryl. Edelson, MD, John Quiles, MD
Brooke Army Medical Center, San Antonio, TX
Introduction: Enterovaginal fistulas are rare, pathologic connections formed usually with underlying inflammatory bowel disease, complicated diverticulitis, radiation therapy, or surgical complications. Symptomatic enterovaginal fistulas commonly present with abnormal passage of stool, flatus, and purulence through the vaginal orifice. Management of these fistulas are complex, prolonged, and multidisciplinary usually resulting in invasive surgery for correction. We present an interesting case of an endoscopic closure of a complex, refractory enterovaginal fistula in a non-surgical candidate.
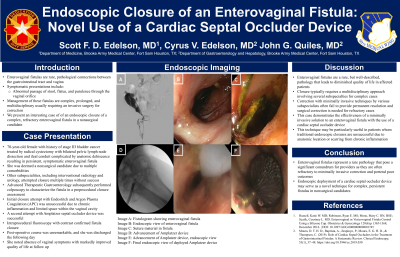
Case Description/Methods: A 70-year-old female with a history of stage III bladder cancer treated by radical cystectomy with bilateral pelvic lymph node dissection and ileal conduit complicated by anastomotic dehiscence resulting in a persistent, symptomatic enterovaginal fistula complicated by recurrent hospitalization, sepsis, and bacterial endocarditis. She was determined to be a non-surgical candidate given comorbid conditions, overall frailty, and the morbidity of the procedure. A multidisciplinary treatment approach was discussed. Interventional radiology attempted closures with the use of a fistula plug twice without success. Advanced gastroenterology subsequently preformed colposcopy to characterize the fistula as a pre-procedural closure assessment. Given the chronic appearance of the fistula tract, initial closure attempt with the use of APC (1L, 60W) combined with endosuturing was unsuccessful due to limited space within the vaginal cavity. A second attempt was performed with successful deployment of an Amplatz septal occluder device as described on Video GIE. Intraprocedural fluoroscopy with contrast confirmed fistula closure. She was discharged the following day with marked improvement in vaginal symptoms. At follow up, she noted continued absence of vaginal symptoms with markedly improved quality of life.
Discussion: Enterocutaneous fistulas represent a rare pathology that pose a significant clinical conundrum for providers as they portend poor outcomes, multiple invasive closure attempts, and poor quality of life. This case demonstrates the effectiveness of a previously described novel approach for management of an enterovaginal fistula with the use of a septal occluder device delivered under endoscopic and fluoroscopic guidance in a non-surgical candidate.

Disclosures:
Scott Edelson, MD, Cyrus Veryl. Edelson, MD, John Quiles, MD. P3764 - Endoscopic Closure of an Enterovaginal Fistula: Novel Use of a Cardiac Septal Occluder Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: Enterovaginal fistulas are rare, pathologic connections formed usually with underlying inflammatory bowel disease, complicated diverticulitis, radiation therapy, or surgical complications. Symptomatic enterovaginal fistulas commonly present with abnormal passage of stool, flatus, and purulence through the vaginal orifice. Management of these fistulas are complex, prolonged, and multidisciplinary usually resulting in invasive surgery for correction. We present an interesting case of an endoscopic closure of a complex, refractory enterovaginal fistula in a non-surgical candidate.
Case Description/Methods: A 70-year-old female with a history of stage III bladder cancer treated by radical cystectomy with bilateral pelvic lymph node dissection and ileal conduit complicated by anastomotic dehiscence resulting in a persistent, symptomatic enterovaginal fistula complicated by recurrent hospitalization, sepsis, and bacterial endocarditis. She was determined to be a non-surgical candidate given comorbid conditions, overall frailty, and the morbidity of the procedure. A multidisciplinary treatment approach was discussed. Interventional radiology attempted closures with the use of a fistula plug twice without success. Advanced gastroenterology subsequently preformed colposcopy to characterize the fistula as a pre-procedural closure assessment. Given the chronic appearance of the fistula tract, initial closure attempt with the use of APC (1L, 60W) combined with endosuturing was unsuccessful due to limited space within the vaginal cavity. A second attempt was performed with successful deployment of an Amplatz septal occluder device as described on Video GIE. Intraprocedural fluoroscopy with contrast confirmed fistula closure. She was discharged the following day with marked improvement in vaginal symptoms. At follow up, she noted continued absence of vaginal symptoms with markedly improved quality of life.
Discussion: Enterocutaneous fistulas represent a rare pathology that pose a significant clinical conundrum for providers as they portend poor outcomes, multiple invasive closure attempts, and poor quality of life. This case demonstrates the effectiveness of a previously described novel approach for management of an enterovaginal fistula with the use of a septal occluder device delivered under endoscopic and fluoroscopic guidance in a non-surgical candidate.

Figure: Fluoroscopic and Endoscopic images of an Enterovaginal fistula prior and after deployment of Cardiac occluder device
Disclosures:
Scott Edelson indicated no relevant financial relationships.
Cyrus Edelson indicated no relevant financial relationships.
John Quiles indicated no relevant financial relationships.
Scott Edelson, MD, Cyrus Veryl. Edelson, MD, John Quiles, MD. P3764 - Endoscopic Closure of an Enterovaginal Fistula: Novel Use of a Cardiac Septal Occluder Device, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
