Tuesday Poster Session
Category: Liver
P3782 - Value of Nutrition and Dietary Support in Alcoholic Hepatitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- KY
Kevin Yang, MD
University at Buffalo
Buffalo, NY
Presenting Author(s)
Kevin Yang, MD, Naren S. Nallapeta, MBBS, Alexander M. Carlson, DO, Nariman Hossein-Javaheri, DO, Brian M. Quigley, PhD, Thomas C. Mahl, MD
University at Buffalo, Buffalo, NY
Introduction: Nutritional status is an often-overlooked component in alcoholic hepatitis. Almost all patients presenting with severe alcoholic hepatitis have a degree of protein calorie malnutrition, which is associated with worse clinical outcomes. Appropriate dietary support in this setting may influence the hospital course.
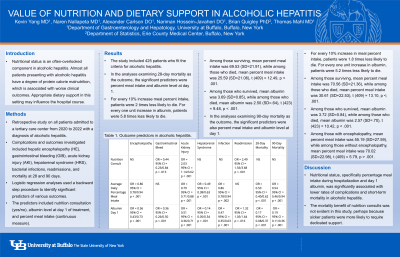
Methods: We designed a retrospective study on all patients admitted to a tertiary care center from 2020 to 2022 with a diagnosis of alcoholic hepatitis. Complications and outcomes investigated included hepatic encephalopathy (HE), gastrointestinal bleeding (GIB), acute kidney injury (AKI), hepatorenal syndrome (HRS), bacterial infections, readmissions, and mortality at 28 and 90 days. We conducted a series of logistic regression analyses using a backward step procedure to identify significant predictors of various outcomes. The predictors included nutrition consultation (yes/no), albumin level at day 1 of treatment, and percent meal intake (continuous measure). Linear regression was also used to analyze the relationship between percent meal intake and the predictors.
Results: The study included 425 patients who fit the criteria for alcoholic hepatitis. In the analysis examining 28-day mortality as the outcome, the significant predictors were percent meal intake and albumin level at day 1. For every 10% increase in meal percent intake, patients were 2 times less likely to die. For every 1 unit increase in albumin, patients were 5.8 times less likely to die. Higher percent meal intake was also a significant predictor for lower rates of HE, AKI, HRS, infection, and 90-day mortality. Higher albumin at day 1 was associated with lower rates of HE, GIB, AKI, HRS, infection, and 90-day mortality, but higher rates of readmission. Nutrition consults were associated with lower rates of GIB (OR = 0.44, 95% CI = 0.23/0.84), higher rates of AKI (OR = 2.03, 95% CI = 1.14/3.62), and more readmissions (OR = 2.49, 95% CI = 1.56/3.68). Patients who received nutrition consultation had higher percentage of meal intake as well (B = 10.51, 95% CI = 5.41/15.62).
Discussion: We found that nutritional status, specifically percentage meal intake during hospitalization and day 1 albumin, was significantly associated with lower rates of complications and short-term mortality in alcoholic hepatitis. The mortality benefit of nutrition consults was not evident in this study, perhaps because sicker patients were more likely to require dedicated support.
Disclosures:
Kevin Yang, MD, Naren S. Nallapeta, MBBS, Alexander M. Carlson, DO, Nariman Hossein-Javaheri, DO, Brian M. Quigley, PhD, Thomas C. Mahl, MD. P3782 - Value of Nutrition and Dietary Support in Alcoholic Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Nutritional status is an often-overlooked component in alcoholic hepatitis. Almost all patients presenting with severe alcoholic hepatitis have a degree of protein calorie malnutrition, which is associated with worse clinical outcomes. Appropriate dietary support in this setting may influence the hospital course.
Methods: We designed a retrospective study on all patients admitted to a tertiary care center from 2020 to 2022 with a diagnosis of alcoholic hepatitis. Complications and outcomes investigated included hepatic encephalopathy (HE), gastrointestinal bleeding (GIB), acute kidney injury (AKI), hepatorenal syndrome (HRS), bacterial infections, readmissions, and mortality at 28 and 90 days. We conducted a series of logistic regression analyses using a backward step procedure to identify significant predictors of various outcomes. The predictors included nutrition consultation (yes/no), albumin level at day 1 of treatment, and percent meal intake (continuous measure). Linear regression was also used to analyze the relationship between percent meal intake and the predictors.
Results: The study included 425 patients who fit the criteria for alcoholic hepatitis. In the analysis examining 28-day mortality as the outcome, the significant predictors were percent meal intake and albumin level at day 1. For every 10% increase in meal percent intake, patients were 2 times less likely to die. For every 1 unit increase in albumin, patients were 5.8 times less likely to die. Higher percent meal intake was also a significant predictor for lower rates of HE, AKI, HRS, infection, and 90-day mortality. Higher albumin at day 1 was associated with lower rates of HE, GIB, AKI, HRS, infection, and 90-day mortality, but higher rates of readmission. Nutrition consults were associated with lower rates of GIB (OR = 0.44, 95% CI = 0.23/0.84), higher rates of AKI (OR = 2.03, 95% CI = 1.14/3.62), and more readmissions (OR = 2.49, 95% CI = 1.56/3.68). Patients who received nutrition consultation had higher percentage of meal intake as well (B = 10.51, 95% CI = 5.41/15.62).
Discussion: We found that nutritional status, specifically percentage meal intake during hospitalization and day 1 albumin, was significantly associated with lower rates of complications and short-term mortality in alcoholic hepatitis. The mortality benefit of nutrition consults was not evident in this study, perhaps because sicker patients were more likely to require dedicated support.
Disclosures:
Kevin Yang indicated no relevant financial relationships.
Naren Nallapeta indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Brian Quigley indicated no relevant financial relationships.
Thomas Mahl indicated no relevant financial relationships.
Kevin Yang, MD, Naren S. Nallapeta, MBBS, Alexander M. Carlson, DO, Nariman Hossein-Javaheri, DO, Brian M. Quigley, PhD, Thomas C. Mahl, MD. P3782 - Value of Nutrition and Dietary Support in Alcoholic Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
