Tuesday Poster Session
Category: Liver
P3783 - Disparity in Orthotopic Liver Transplant Listing With Respect to Race and Access to Care: An Analysis of the National Inpatient Sample 2016-2020
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Christopher Chhoun, DO
Jefferson Health
Cherry Hill, New Jersey
Presenting Author(s)
Award: ACG Governors Award for Excellence in Clinical Research (Trainee)
Award: Presidential Poster Award
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Nielsen Gabriel, DO3, Marisa Pope, DO4, Neethi Dasu, DO5, Yaser Khalid, DO6, Jonathan Foster, DO1, Kwan Lau, MD3
1Jefferson Health, Cherry Hill, NJ; 2University of Pennsylvania, Philadelphia, PA; 3Temple University Hospital, Philadelphia, PA; 4Jefferson Health, Stratford, NJ; 5Jefferson Health, New Jersey, NJ; 6Wright Center for GME/Geisinger Health System, Scranton, PA
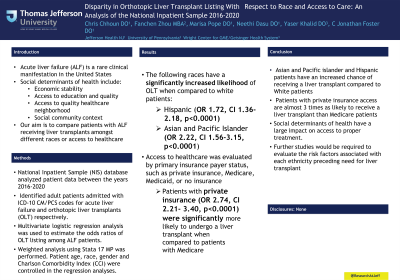
Introduction: Acute liver failure (ALF) is a rare clinical manifestation in the United States.
Social determinants of health consist of a person’s economic stability, access to education and quality, access to quality healthcare, neighborhood, and social community context. The differences between each of the factors cause great inequity within healthcare. We hypothesize that patients with ALF that receive liver transplants are not equal among different races or access to healthcare.
Methods: The National Inpatient Sample (NIS) database (2016-2020) was analyzed to identify adult patients admitted with ICD-10 CM/PCS codes for acute liver failure and orthotopic liver transplants (OLT) respectively. Multivariate logistic regression analysis was used to estimate the odds ratios of OLT listing among ALF patients. Weighted analysis using Stata 17 MP was performed. Patient age, race, gender and Charlson Comorbidity Index (CCI) were controlled in the regression analyses.
Results: Our study showed a significantly increased likelihood of OLT amongst Hispanic (OR 1.72, CI 1.36-2.18, p< 0.0001) and Asian and Pacific Islander (OR 2.22, CI 1.56-3.15, p< 0.0001) patients compared to white patients. In addition, access to healthcare was evaluated by primary insurance payer status, such as private insurance, medicare, medicaid, or no insurance. Our analysis showed that patients with private insurance (OR 2.74, CI 2.21- 3.40, p< 0.0001) were significantly more likely to undergo a liver transplant.
Discussion: Asian and Pacific islander and Hispanic patients have an increased chance of receiving a liver transplant compared to White patients. In addition, patients with private insurance access are almost 3 times as likely to receive a liver transplant as Medicare patients. Social determinants of health have a large impact on access to proper treatment. However, this data is limited and further studies would be required to evaluate the risk factors associated with each ethnicity preceding need for liver transplant.
Disclosures:
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Nielsen Gabriel, DO3, Marisa Pope, DO4, Neethi Dasu, DO5, Yaser Khalid, DO6, Jonathan Foster, DO1, Kwan Lau, MD3. P3783 - Disparity in Orthotopic Liver Transplant Listing With Respect to Race and Access to Care: An Analysis of the National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Award: Presidential Poster Award
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Nielsen Gabriel, DO3, Marisa Pope, DO4, Neethi Dasu, DO5, Yaser Khalid, DO6, Jonathan Foster, DO1, Kwan Lau, MD3
1Jefferson Health, Cherry Hill, NJ; 2University of Pennsylvania, Philadelphia, PA; 3Temple University Hospital, Philadelphia, PA; 4Jefferson Health, Stratford, NJ; 5Jefferson Health, New Jersey, NJ; 6Wright Center for GME/Geisinger Health System, Scranton, PA
Introduction: Acute liver failure (ALF) is a rare clinical manifestation in the United States.
Social determinants of health consist of a person’s economic stability, access to education and quality, access to quality healthcare, neighborhood, and social community context. The differences between each of the factors cause great inequity within healthcare. We hypothesize that patients with ALF that receive liver transplants are not equal among different races or access to healthcare.
Methods: The National Inpatient Sample (NIS) database (2016-2020) was analyzed to identify adult patients admitted with ICD-10 CM/PCS codes for acute liver failure and orthotopic liver transplants (OLT) respectively. Multivariate logistic regression analysis was used to estimate the odds ratios of OLT listing among ALF patients. Weighted analysis using Stata 17 MP was performed. Patient age, race, gender and Charlson Comorbidity Index (CCI) were controlled in the regression analyses.
Results: Our study showed a significantly increased likelihood of OLT amongst Hispanic (OR 1.72, CI 1.36-2.18, p< 0.0001) and Asian and Pacific Islander (OR 2.22, CI 1.56-3.15, p< 0.0001) patients compared to white patients. In addition, access to healthcare was evaluated by primary insurance payer status, such as private insurance, medicare, medicaid, or no insurance. Our analysis showed that patients with private insurance (OR 2.74, CI 2.21- 3.40, p< 0.0001) were significantly more likely to undergo a liver transplant.
Discussion: Asian and Pacific islander and Hispanic patients have an increased chance of receiving a liver transplant compared to White patients. In addition, patients with private insurance access are almost 3 times as likely to receive a liver transplant as Medicare patients. Social determinants of health have a large impact on access to proper treatment. However, this data is limited and further studies would be required to evaluate the risk factors associated with each ethnicity preceding need for liver transplant.
Disclosures:
Christopher Chhoun indicated no relevant financial relationships.
Fanchen Zhou indicated no relevant financial relationships.
Nielsen Gabriel indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Yaser Khalid indicated no relevant financial relationships.
Jonathan Foster: Conmed – Consultant. Steris – Consultant.
Kwan Lau indicated no relevant financial relationships.
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Nielsen Gabriel, DO3, Marisa Pope, DO4, Neethi Dasu, DO5, Yaser Khalid, DO6, Jonathan Foster, DO1, Kwan Lau, MD3. P3783 - Disparity in Orthotopic Liver Transplant Listing With Respect to Race and Access to Care: An Analysis of the National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

