Tuesday Poster Session
Category: Liver
P3785 - NASH and Primary Insurance Payer as Independent Predictors of Inpatient Clinical Outcomes in Acute Mesenteric Ischemia - An Analysis of the National Inpatient Sample 2016-2020
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Christopher Chhoun, DO
Jefferson Health
Cherry Hill, New Jersey
Presenting Author(s)
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Neethi Dasu, DO3, Nielsen Gabriel, DO4, Marisa Pope, DO5, Jonathan Foster, DO1, Lucy Joo, DO1
1Jefferson Health, Cherry Hill, NJ; 2University of Pennsylvania, Philadelphia, PA; 3Jefferson Health, New Jersey, NJ; 4Temple University Hospital, Philadelphia, PA; 5Jefferson Health, Stratford, NJ
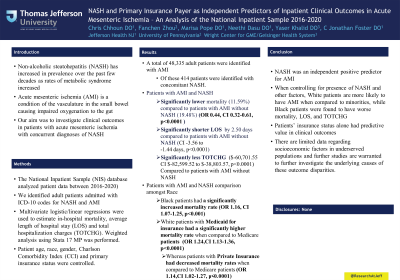
Introduction: Non-Alcoholic Steatohepatitis (NASH) has increased in prevalence over the past few decades as rates of metabolic syndrome have increased. Acute mesenteric ischemia (AMI) is a condition of the vasculature in the small bowel causing impaired oxygenation to the gut. This disease process is associated with high mortality rates. Our aim was to investigate clinical outcomes in patients with acute mesenteric ischemia with concurrent diagnoses of NASH.
Methods: The National Inpatient Sample (NIS) database (2016-2020) was analyzed to identify adult patients admitted with ICD-10 codes for NASH and AMI. Multivariate logistic/linear regressions were used to estimate in-hospital mortality, average length of hospital stay (LOS) and total hospitalization charges (TOTCHG). Weighted analysis using Stata 17 MP was performed. Patient age, race, gender, Charlson Comorbidity Index (CCI) and primary insurance status were controlled.
Results: A total of 48,335 adult patients were identified with AMI. Of these, 414 patients were identified with concomitant NASH.
We found that patients with AMI and concurrent NASH had a significant lower inpatient mortality (OR 0.44, CI 0.32-0.61, p< 0.0001), averaging 11.59%, compared with AMI patients without concurrent NASH, averaging 19.48%, assuming the same age, gender, race, primary insurance payer, and CCI. Meanwhile, they also had a shorter LOS (-2.50 days,CI -3.56 to -1.44 days, p< 0.0001) and decreased TOTCHG ($-60,701.55, CI $-82,599.52 to $-38,803.57, p< 0.0001).
Additionally, assuming other factors equal, Black patients had a significantly increased mortality (OR 1.16, CI 1.07-1.25, p< 0.001) vs. White patients; compared with Medicare patients, Medicaid patients had a significantly higher mortality (OR 1.24,CI 1.13-1.36, p< 0.0001) whereas patients with private insurance had a decreased mortality (OR 1.14,CI 1.02-1.27, p< 0.0001).
Discussion: We found that NASH was an independent positive predictor for AMI. When controlling for presence of NASH and other factors, White patients are more likely to have AMI when compared to minorities, while Black patients were found to have worse mortality, LOS, and TOTCHG. Furthermore,we found that patients’ insurance status alone had predictive value in clinical outcomes. There are limited data regarding socioeconomic factors in underserved populations and further studies are warranted to further investigate the underlying causes of these outcome disparities.
Disclosures:
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Neethi Dasu, DO3, Nielsen Gabriel, DO4, Marisa Pope, DO5, Jonathan Foster, DO1, Lucy Joo, DO1. P3785 - NASH and Primary Insurance Payer as Independent Predictors of Inpatient Clinical Outcomes in Acute Mesenteric Ischemia - An Analysis of the National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Jefferson Health, Cherry Hill, NJ; 2University of Pennsylvania, Philadelphia, PA; 3Jefferson Health, New Jersey, NJ; 4Temple University Hospital, Philadelphia, PA; 5Jefferson Health, Stratford, NJ
Introduction: Non-Alcoholic Steatohepatitis (NASH) has increased in prevalence over the past few decades as rates of metabolic syndrome have increased. Acute mesenteric ischemia (AMI) is a condition of the vasculature in the small bowel causing impaired oxygenation to the gut. This disease process is associated with high mortality rates. Our aim was to investigate clinical outcomes in patients with acute mesenteric ischemia with concurrent diagnoses of NASH.
Methods: The National Inpatient Sample (NIS) database (2016-2020) was analyzed to identify adult patients admitted with ICD-10 codes for NASH and AMI. Multivariate logistic/linear regressions were used to estimate in-hospital mortality, average length of hospital stay (LOS) and total hospitalization charges (TOTCHG). Weighted analysis using Stata 17 MP was performed. Patient age, race, gender, Charlson Comorbidity Index (CCI) and primary insurance status were controlled.
Results: A total of 48,335 adult patients were identified with AMI. Of these, 414 patients were identified with concomitant NASH.
We found that patients with AMI and concurrent NASH had a significant lower inpatient mortality (OR 0.44, CI 0.32-0.61, p< 0.0001), averaging 11.59%, compared with AMI patients without concurrent NASH, averaging 19.48%, assuming the same age, gender, race, primary insurance payer, and CCI. Meanwhile, they also had a shorter LOS (-2.50 days,CI -3.56 to -1.44 days, p< 0.0001) and decreased TOTCHG ($-60,701.55, CI $-82,599.52 to $-38,803.57, p< 0.0001).
Additionally, assuming other factors equal, Black patients had a significantly increased mortality (OR 1.16, CI 1.07-1.25, p< 0.001) vs. White patients; compared with Medicare patients, Medicaid patients had a significantly higher mortality (OR 1.24,CI 1.13-1.36, p< 0.0001) whereas patients with private insurance had a decreased mortality (OR 1.14,CI 1.02-1.27, p< 0.0001).
Discussion: We found that NASH was an independent positive predictor for AMI. When controlling for presence of NASH and other factors, White patients are more likely to have AMI when compared to minorities, while Black patients were found to have worse mortality, LOS, and TOTCHG. Furthermore,we found that patients’ insurance status alone had predictive value in clinical outcomes. There are limited data regarding socioeconomic factors in underserved populations and further studies are warranted to further investigate the underlying causes of these outcome disparities.
Disclosures:
Christopher Chhoun indicated no relevant financial relationships.
Fanchen Zhou indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Nielsen Gabriel indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
Jonathan Foster: Conmed – Consultant. Steris – Consultant.
Lucy Joo indicated no relevant financial relationships.
Christopher Chhoun, DO1, Fanchen Zhou, MBA2, Neethi Dasu, DO3, Nielsen Gabriel, DO4, Marisa Pope, DO5, Jonathan Foster, DO1, Lucy Joo, DO1. P3785 - NASH and Primary Insurance Payer as Independent Predictors of Inpatient Clinical Outcomes in Acute Mesenteric Ischemia - An Analysis of the National Inpatient Sample 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
