Tuesday Poster Session
Category: Liver
P3787 - The Effect of Cocaine Use on Patient Outcomes in Those Evaluated for Liver Transplant
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Darya M. Herscovici, BS
UMass Chan Medical School
Worcester, MA
Presenting Author(s)
Darya M. Herscovici, BS, Katherine M.. Cooper, MD, Alessandro Colletta, MD, Deepika Devuni, MD
UMass Chan Medical School, Worcester, MA
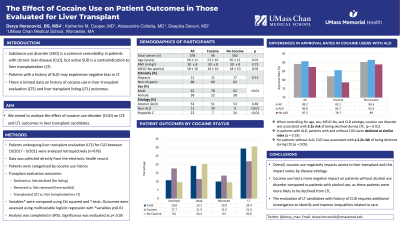
Introduction: Substance use disorder (SUD) is a common comorbidity in patients with chronic liver disease (CLD). Active SUD is a contraindication in most scenarios related to liver transplantation (LT). However, it is possible that patients with a history of SUD experience negative bias in LT. Currently, there is limited data on history of cocaine use in liver transplant evaluation (LTE) and liver transplant listing (LTL) outcomes. We aimed to analyze the effect of cocaine use disorder (CUD) on LTE and LTL outcomes in liver transplant candidates.
Methods: We completed a single center retrospective analysis of patients undergoing LTE for evaluation over a 4-year period. Patients evaluated for CLD were included; patients with acute liver failure and prior LT were excluded. Substance use history was during the TLE psychosocial assessment. CUD was defined as current or prior regular use of cocaine. Outcomes of LTE included declined vs. not declined for listing. Data was compared using chi squared and t tests. The relationship between CUD and outcomes was assessed using univariate logistic regression and further analyzed with a parsimonious multivariate model. Analysis was completed in SPSS software. Significance was determined as p< 0.05.
Results: 678 patients were included, of which 96 (14%) patients reported current or past cocaine use. Usage was highest in hepatitis C cirrhosis (HCV) and alcohol liver disease (ALD) where 42% and 14% reported CUD, respectively. Patients with CUD were younger (p=0.01), had a lower MELD score (p=0.02), and more likely to be male (p< 0.01). More patients with CUD were declined during LTE compared to no CUD (18% vs. 10%,, p = .02). When controlling for age, sex, MELD, and CLD etiology, CUD was associated with 2.2 x risk of being declined during LTE (p< 0.014). In patients with ALD, patients with and without CUD were declined at similar rates (14% vs. 8%, p=0.18). However, in patients without ALD, CUD was associated with a 2.2 x risk of being declined during LTE (p = 0.05).
Discussion: Our results suggest CUD negatively impacts access to liver transplant. However, this impact varies by disease etiology. For example, we found CUD had a more negative impact on patients without alcohol use disorder compared to patients with solely cocaine use as these patients were more likely to be declined from liver transplant listing. The evaluation of liver transplant candidates with a history of CUD requires additional investigation to identify and improve inequalities related to care.
Disclosures:
Darya M. Herscovici, BS, Katherine M.. Cooper, MD, Alessandro Colletta, MD, Deepika Devuni, MD. P3787 - The Effect of Cocaine Use on Patient Outcomes in Those Evaluated for Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
UMass Chan Medical School, Worcester, MA
Introduction: Substance use disorder (SUD) is a common comorbidity in patients with chronic liver disease (CLD). Active SUD is a contraindication in most scenarios related to liver transplantation (LT). However, it is possible that patients with a history of SUD experience negative bias in LT. Currently, there is limited data on history of cocaine use in liver transplant evaluation (LTE) and liver transplant listing (LTL) outcomes. We aimed to analyze the effect of cocaine use disorder (CUD) on LTE and LTL outcomes in liver transplant candidates.
Methods: We completed a single center retrospective analysis of patients undergoing LTE for evaluation over a 4-year period. Patients evaluated for CLD were included; patients with acute liver failure and prior LT were excluded. Substance use history was during the TLE psychosocial assessment. CUD was defined as current or prior regular use of cocaine. Outcomes of LTE included declined vs. not declined for listing. Data was compared using chi squared and t tests. The relationship between CUD and outcomes was assessed using univariate logistic regression and further analyzed with a parsimonious multivariate model. Analysis was completed in SPSS software. Significance was determined as p< 0.05.
Results: 678 patients were included, of which 96 (14%) patients reported current or past cocaine use. Usage was highest in hepatitis C cirrhosis (HCV) and alcohol liver disease (ALD) where 42% and 14% reported CUD, respectively. Patients with CUD were younger (p=0.01), had a lower MELD score (p=0.02), and more likely to be male (p< 0.01). More patients with CUD were declined during LTE compared to no CUD (18% vs. 10%,, p = .02). When controlling for age, sex, MELD, and CLD etiology, CUD was associated with 2.2 x risk of being declined during LTE (p< 0.014). In patients with ALD, patients with and without CUD were declined at similar rates (14% vs. 8%, p=0.18). However, in patients without ALD, CUD was associated with a 2.2 x risk of being declined during LTE (p = 0.05).
Discussion: Our results suggest CUD negatively impacts access to liver transplant. However, this impact varies by disease etiology. For example, we found CUD had a more negative impact on patients without alcohol use disorder compared to patients with solely cocaine use as these patients were more likely to be declined from liver transplant listing. The evaluation of liver transplant candidates with a history of CUD requires additional investigation to identify and improve inequalities related to care.
Disclosures:
Darya Herscovici indicated no relevant financial relationships.
Katherine Cooper indicated no relevant financial relationships.
Alessandro Colletta indicated no relevant financial relationships.
Deepika Devuni: NIAAA (AA017986) – Grant/Research Support. Sequana Medical – Grant/Research Support.
Darya M. Herscovici, BS, Katherine M.. Cooper, MD, Alessandro Colletta, MD, Deepika Devuni, MD. P3787 - The Effect of Cocaine Use on Patient Outcomes in Those Evaluated for Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
