Tuesday Poster Session
Category: Liver
P3790 - Cirrhotics Who Receive Palliative Care Consultation Are Less Likely to Undergo Transfusions and Procedures; More Likely to Die in Hospital
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Taimur S. Muzammil, MD
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Taimur S. Muzammil, MD1, Yue Yin, PhD2, Michael Babich, MD1, Jose Oliva, MD1, Nabeeha Mohy-ud-din, MD1
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny Singer Research Institute, Allegheny Health Network, Pittsburgh, PA
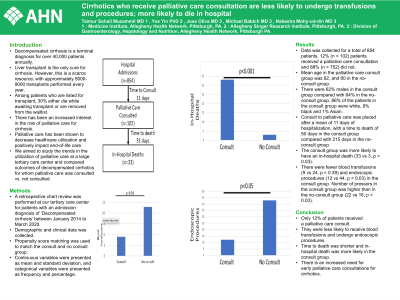
Introduction: Decompensated cirrhosis is a terminal diagnosis for over 40,000 patients annually. Liver transplant is the only cure for cirrhosis. However, this is a scarce resource, with approximately 8000-9000 transplants performed every year. Among patients who are listed for transplant, 30% either die while awaiting transplant or are removed from the wait list. There has been an increased interest in the role of palliative care for cirrhosis. Palliative care has been shown to decrease health care utilization and positively impact end-of-life care. We aimed to study the trends in utilization of palliative care at a large tertiary care center and compared outcomes of decompensated cirrhotics for whom palliative care was consulted vs. not consulted.
Methods: A retrospective chart review for patients with an admission diagnosis of ‘Decompensated cirrhosis’ between January 2014 to March 2020 was performed at our tertiary care center. Demographic and clinical data was collected. Propensity score matching was used to match the consult and no consult group. Continuous variables were presented as mean and standard deviation, categorical variables were presented as frequency and percentage.
Results: Data was collected for a total of 854 patients. 12% (n = 102) patients received a palliative care consultation and 88% (n = 752) did not. Mean age in the palliative care consult group was 62, and 60 in the no-consult group. There were 62% males in the consult group compared with 64% in the no-consult group. 86% of the patients in the consult group were white, 9% black and 1% Asian.
Consult to palliative care was placed after a mean of 11 days of hospitalization, with a time to death of 50 days in the consult group compared with 215 days in the no-consult group. The consult group was more likely to have an in-hospital death (33 vs 3, p < 0.03). There were fewer blood transfusions (9 vs 24, p = 0.39) and endoscopic procedures (12 vs 44, p < 0.03) in the consult group. Number of pressors in the consult group was higher than in the no-consult group (22 vs 16, p < 0.03).
Discussion: Only 12% of patients received a palliative care consult. They were less likely to receive blood transfusions and undergo endoscopic procedures. Time to death was shorter and in-hospital death was more likely in the consult group. There is an increased need for early palliative care consultations for cirrhotics.

Disclosures:
Taimur S. Muzammil, MD1, Yue Yin, PhD2, Michael Babich, MD1, Jose Oliva, MD1, Nabeeha Mohy-ud-din, MD1. P3790 - Cirrhotics Who Receive Palliative Care Consultation Are Less Likely to Undergo Transfusions and Procedures; More Likely to Die in Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny Singer Research Institute, Allegheny Health Network, Pittsburgh, PA
Introduction: Decompensated cirrhosis is a terminal diagnosis for over 40,000 patients annually. Liver transplant is the only cure for cirrhosis. However, this is a scarce resource, with approximately 8000-9000 transplants performed every year. Among patients who are listed for transplant, 30% either die while awaiting transplant or are removed from the wait list. There has been an increased interest in the role of palliative care for cirrhosis. Palliative care has been shown to decrease health care utilization and positively impact end-of-life care. We aimed to study the trends in utilization of palliative care at a large tertiary care center and compared outcomes of decompensated cirrhotics for whom palliative care was consulted vs. not consulted.
Methods: A retrospective chart review for patients with an admission diagnosis of ‘Decompensated cirrhosis’ between January 2014 to March 2020 was performed at our tertiary care center. Demographic and clinical data was collected. Propensity score matching was used to match the consult and no consult group. Continuous variables were presented as mean and standard deviation, categorical variables were presented as frequency and percentage.
Results: Data was collected for a total of 854 patients. 12% (n = 102) patients received a palliative care consultation and 88% (n = 752) did not. Mean age in the palliative care consult group was 62, and 60 in the no-consult group. There were 62% males in the consult group compared with 64% in the no-consult group. 86% of the patients in the consult group were white, 9% black and 1% Asian.
Consult to palliative care was placed after a mean of 11 days of hospitalization, with a time to death of 50 days in the consult group compared with 215 days in the no-consult group. The consult group was more likely to have an in-hospital death (33 vs 3, p < 0.03). There were fewer blood transfusions (9 vs 24, p = 0.39) and endoscopic procedures (12 vs 44, p < 0.03) in the consult group. Number of pressors in the consult group was higher than in the no-consult group (22 vs 16, p < 0.03).
Discussion: Only 12% of patients received a palliative care consult. They were less likely to receive blood transfusions and undergo endoscopic procedures. Time to death was shorter and in-hospital death was more likely in the consult group. There is an increased need for early palliative care consultations for cirrhotics.

Figure: Image 1
Disclosures:
Taimur Muzammil indicated no relevant financial relationships.
Yue Yin indicated no relevant financial relationships.
Michael Babich indicated no relevant financial relationships.
Jose Oliva indicated no relevant financial relationships.
Nabeeha Mohy-ud-din indicated no relevant financial relationships.
Taimur S. Muzammil, MD1, Yue Yin, PhD2, Michael Babich, MD1, Jose Oliva, MD1, Nabeeha Mohy-ud-din, MD1. P3790 - Cirrhotics Who Receive Palliative Care Consultation Are Less Likely to Undergo Transfusions and Procedures; More Likely to Die in Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
