Tuesday Poster Session
Category: Liver
P3795 - Impact of Availability of Primary Care Physicians and Racial Disparities in Hepatocellular Carcinoma-Related Mortality in the United States
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Daniyal Raza, MD
LSU Health Sciences Center
Shreveport, LA
Presenting Author(s)
Daniyal Raza, MD1, Syed Musa Raza, MD1, Maryam Mubashir, MD1, Subash Garikipathi, MD2, Udhayvyir Grewal, MD3
1LSU Health Sciences Center, Shreveport, LA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3University of Iowa Hospitals & Clinics, Iowa City, OH
Introduction: Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide. Five-year survival of HCC is 18%, which is second only to pancreatic cancer. Consistent screening directed by primary care physicians (PCPs) is vital to reduce HCC-related mortality among at-risk populations through active surveillance. However, the impact of access to primary care on HCC-related mortality is not well studied.
Methods: We extracted data on crude incidence of hepatocellular carcinoma among all 50 states and District of Columbia (D.C.) from the Center for Disease Control (CDC) WONDER database for the year 2019. Data on number of actively practicing PCPs in all 50 states and D.C. were obtained from Association of American Medical Colleges (AAMC) 2021 State Physician Workforce Data Report (for the year 2020). We studied the correlation between the ratio of number of PCPs per HCC case with age-adjusted mortality rate (AAMR) of HCC among all states except Nevada. We studied the correlation between the ratio of PCPs per HCC case with AAMR of HCC among Caucasian and AA populations for 31 states (due to missing data). Pearson’s co-efficient was used to study correlations and T-test was used for comparing independent samples. Statistical analysis was performed using Vassar Stats.
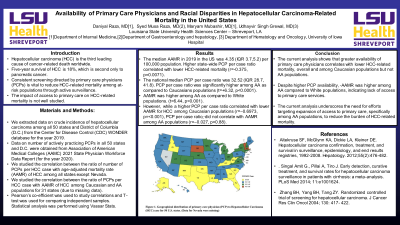
Results: The median AAMR in 2019 in the US was 4.35 (IQR 3.7,5.2) per 100,000 population. Higher state-wide PCP per case ratio correlated with lower HCC-related mortality (r=-0.375, p=0.0071). The national median PCP per case ratio was 32.52 (IQR 28.7, 41.8). PCP per case ratio was significantly higher among AA as compared to Caucasians populations (t=+6.32, p< 0.0001). AAMR was higher among AA as compared to White populations. (t=6.44, p< 0.001). However, while a higher PCP per case ratio correlated with lower AAMR for HCC among Caucasian populations (r=–0.6973, p=< 0.001), PCP per case ratio did not corelate with AAMR among AA populations (r=–0.027, p=0.88).
Discussion: The current analysis shows that greater availability of primary care physicians correlates with lower HCC-related mortality, overall and among Caucasian populations but not AA populations. Despite higher PCP availability, AAMR was higher among AA compared to White populations, indicating lack of access to primary care services. The current analysis underscores the need for efforts targeting expansion of access to primary care, specifically among AA populations, to reduce the burden of HCC-related mortality.

Disclosures:
Daniyal Raza, MD1, Syed Musa Raza, MD1, Maryam Mubashir, MD1, Subash Garikipathi, MD2, Udhayvyir Grewal, MD3. P3795 - Impact of Availability of Primary Care Physicians and Racial Disparities in Hepatocellular Carcinoma-Related Mortality in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1LSU Health Sciences Center, Shreveport, LA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3University of Iowa Hospitals & Clinics, Iowa City, OH
Introduction: Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide. Five-year survival of HCC is 18%, which is second only to pancreatic cancer. Consistent screening directed by primary care physicians (PCPs) is vital to reduce HCC-related mortality among at-risk populations through active surveillance. However, the impact of access to primary care on HCC-related mortality is not well studied.
Methods: We extracted data on crude incidence of hepatocellular carcinoma among all 50 states and District of Columbia (D.C.) from the Center for Disease Control (CDC) WONDER database for the year 2019. Data on number of actively practicing PCPs in all 50 states and D.C. were obtained from Association of American Medical Colleges (AAMC) 2021 State Physician Workforce Data Report (for the year 2020). We studied the correlation between the ratio of number of PCPs per HCC case with age-adjusted mortality rate (AAMR) of HCC among all states except Nevada. We studied the correlation between the ratio of PCPs per HCC case with AAMR of HCC among Caucasian and AA populations for 31 states (due to missing data). Pearson’s co-efficient was used to study correlations and T-test was used for comparing independent samples. Statistical analysis was performed using Vassar Stats.
Results: The median AAMR in 2019 in the US was 4.35 (IQR 3.7,5.2) per 100,000 population. Higher state-wide PCP per case ratio correlated with lower HCC-related mortality (r=-0.375, p=0.0071). The national median PCP per case ratio was 32.52 (IQR 28.7, 41.8). PCP per case ratio was significantly higher among AA as compared to Caucasians populations (t=+6.32, p< 0.0001). AAMR was higher among AA as compared to White populations. (t=6.44, p< 0.001). However, while a higher PCP per case ratio correlated with lower AAMR for HCC among Caucasian populations (r=–0.6973, p=< 0.001), PCP per case ratio did not corelate with AAMR among AA populations (r=–0.027, p=0.88).
Discussion: The current analysis shows that greater availability of primary care physicians correlates with lower HCC-related mortality, overall and among Caucasian populations but not AA populations. Despite higher PCP availability, AAMR was higher among AA compared to White populations, indicating lack of access to primary care services. The current analysis underscores the need for efforts targeting expansion of access to primary care, specifically among AA populations, to reduce the burden of HCC-related mortality.

Figure: Geographical distribution of primary care physician (PCP) per Hepatocellular Carcinoma (HCC) case ratios for all 50 U.S. states. (Data for Nevada were missing)
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Syed Musa Raza indicated no relevant financial relationships.
Maryam Mubashir indicated no relevant financial relationships.
Subash Garikipathi indicated no relevant financial relationships.
Udhayvyir Grewal indicated no relevant financial relationships.
Daniyal Raza, MD1, Syed Musa Raza, MD1, Maryam Mubashir, MD1, Subash Garikipathi, MD2, Udhayvyir Grewal, MD3. P3795 - Impact of Availability of Primary Care Physicians and Racial Disparities in Hepatocellular Carcinoma-Related Mortality in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
