Tuesday Poster Session
Category: Liver
P3807 - The Risk of Hypertensive Disorders of Pregnancy Is Not Increased Among Individuals with Non-Alcoholic Fatty Liver Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Lindsay M. Clarke, MD, MS
Brigham and Women's Hospital
Boston, MA
Presenting Author(s)
Lindsay M. Clarke, MD, MS1, Daryl Selen, MD2, Carolin Schulte, PhD3, Tanayott Thaweethai, PhD3, Sarah Hsu, MS3, Chu Yu, MS3, Kaitlyn James, PhD3, Adam Buckholz, MD4, John G. Ilagan, MD, MSc5, Sonal Kumar, MD4, Camille Powe, MD3
1Brigham and Women's Hospital, Boston, MA; 2Brown Rhode Island Hospital, Providence, RI; 3Massachusetts General Hospital, Boston, MA; 4New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 5New York Presbyterian-Columbia, New York, NY
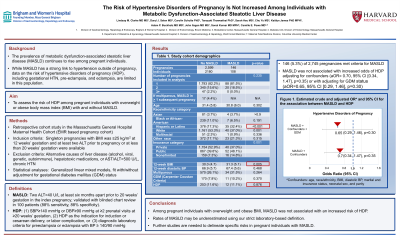
Introduction: The prevalence of non-alcoholic fatty liver disease (NAFLD) continues to rise among pregnant individuals. While NAFLD has a strong link to hypertension outside of pregnancy, data on the risk of hypertensive disorders of pregnancy (HDP) in NAFLD are limited. Among pregnant individuals with overweight or obese body mass index (BMI), we aimed to compare the risk of HDP in those with and without NAFLD.
Methods: We performed a retrospective cohort study of pregnancies cared for at a US academic center from 1998 to 2016. Singleton pregnancies were included if BMI was ≥25 kg/m2 at 12 weeks’ gestation and at least two ALT prior to pregnancy or at less than 20 weeks’ gestation were available. After excluding individuals with alternative causes of liver disease (alcohol, viral, genetic, autoimmune), hepatotoxic medications, or AST/ALT >500 U/L, we defined NAFLD as two ALT >40 U/L at least six months apart prior to 20 weeks’ gestation in the index pregnancy. This NAFLD definition was validated with blinded chart review in 100 patients (88% sensitivity, 88% specificity). The primary outcome was HDP (defined using outpatient blood pressures and labor and delivery records). Generalized linear mixed models examined the association between NAFLD and HDP, adjusting for age, race/ethnicity, BMI, diastolic BP, marital and insurance status, neonatal sex, and parity. Models were fit with/without adjustment for gestational diabetes mellitus (GDM) status.
Results: Of the 2,745 pregnancies (2,288 individuals) included, 146 (5.3%) met criteria for NAFLD. Those with NAFLD had higher BMI at 12 weeks’ gestation (mean of 31.3 kg/m2 vs. 30.0 in non-NAFLD, p=0.005), were more likely to be Hispanic/Latina (32.4% vs. 17.3%, p< 0.001), and were more likely to have public health insurance (48.1% vs. 39.8%, p=0.001). Age and diastolic BP were similar between both groups. Comparing NAFLD with non-NAFLD pregnancies, the rate of HDP was 11.1% vs. 11.6% (p=0.876). NAFLD was not associated with increased odds of HDP in adjusted models (adjusted odds ratio [aOR]= 0.70, 95% CI [0.34, 1.47], p=0.35). Adjusting for GDM status did not change the results (aOR=0.65, 95% CI [0.29, 1.46], p=0.30).
Discussion: Among pregnant individuals with overweight and obese BMI, NAFLD was not associated with an increased risk of HDP. Rates of NAFLD may be underestimated using our strict laboratory-based definition. Further studies are needed to delineate specific risks in pregnant individuals with NAFLD.
Disclosures:
Lindsay M. Clarke, MD, MS1, Daryl Selen, MD2, Carolin Schulte, PhD3, Tanayott Thaweethai, PhD3, Sarah Hsu, MS3, Chu Yu, MS3, Kaitlyn James, PhD3, Adam Buckholz, MD4, John G. Ilagan, MD, MSc5, Sonal Kumar, MD4, Camille Powe, MD3. P3807 - The Risk of Hypertensive Disorders of Pregnancy Is Not Increased Among Individuals with Non-Alcoholic Fatty Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Brown Rhode Island Hospital, Providence, RI; 3Massachusetts General Hospital, Boston, MA; 4New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 5New York Presbyterian-Columbia, New York, NY
Introduction: The prevalence of non-alcoholic fatty liver disease (NAFLD) continues to rise among pregnant individuals. While NAFLD has a strong link to hypertension outside of pregnancy, data on the risk of hypertensive disorders of pregnancy (HDP) in NAFLD are limited. Among pregnant individuals with overweight or obese body mass index (BMI), we aimed to compare the risk of HDP in those with and without NAFLD.
Methods: We performed a retrospective cohort study of pregnancies cared for at a US academic center from 1998 to 2016. Singleton pregnancies were included if BMI was ≥25 kg/m2 at 12 weeks’ gestation and at least two ALT prior to pregnancy or at less than 20 weeks’ gestation were available. After excluding individuals with alternative causes of liver disease (alcohol, viral, genetic, autoimmune), hepatotoxic medications, or AST/ALT >500 U/L, we defined NAFLD as two ALT >40 U/L at least six months apart prior to 20 weeks’ gestation in the index pregnancy. This NAFLD definition was validated with blinded chart review in 100 patients (88% sensitivity, 88% specificity). The primary outcome was HDP (defined using outpatient blood pressures and labor and delivery records). Generalized linear mixed models examined the association between NAFLD and HDP, adjusting for age, race/ethnicity, BMI, diastolic BP, marital and insurance status, neonatal sex, and parity. Models were fit with/without adjustment for gestational diabetes mellitus (GDM) status.
Results: Of the 2,745 pregnancies (2,288 individuals) included, 146 (5.3%) met criteria for NAFLD. Those with NAFLD had higher BMI at 12 weeks’ gestation (mean of 31.3 kg/m2 vs. 30.0 in non-NAFLD, p=0.005), were more likely to be Hispanic/Latina (32.4% vs. 17.3%, p< 0.001), and were more likely to have public health insurance (48.1% vs. 39.8%, p=0.001). Age and diastolic BP were similar between both groups. Comparing NAFLD with non-NAFLD pregnancies, the rate of HDP was 11.1% vs. 11.6% (p=0.876). NAFLD was not associated with increased odds of HDP in adjusted models (adjusted odds ratio [aOR]= 0.70, 95% CI [0.34, 1.47], p=0.35). Adjusting for GDM status did not change the results (aOR=0.65, 95% CI [0.29, 1.46], p=0.30).
Discussion: Among pregnant individuals with overweight and obese BMI, NAFLD was not associated with an increased risk of HDP. Rates of NAFLD may be underestimated using our strict laboratory-based definition. Further studies are needed to delineate specific risks in pregnant individuals with NAFLD.
Disclosures:
Lindsay Clarke indicated no relevant financial relationships.
Daryl Selen indicated no relevant financial relationships.
Carolin Schulte indicated no relevant financial relationships.
Tanayott Thaweethai indicated no relevant financial relationships.
Sarah Hsu indicated no relevant financial relationships.
Chu Yu indicated no relevant financial relationships.
Kaitlyn James indicated no relevant financial relationships.
Adam Buckholz indicated no relevant financial relationships.
John Ilagan indicated no relevant financial relationships.
Sonal Kumar indicated no relevant financial relationships.
Camille Powe indicated no relevant financial relationships.
Lindsay M. Clarke, MD, MS1, Daryl Selen, MD2, Carolin Schulte, PhD3, Tanayott Thaweethai, PhD3, Sarah Hsu, MS3, Chu Yu, MS3, Kaitlyn James, PhD3, Adam Buckholz, MD4, John G. Ilagan, MD, MSc5, Sonal Kumar, MD4, Camille Powe, MD3. P3807 - The Risk of Hypertensive Disorders of Pregnancy Is Not Increased Among Individuals with Non-Alcoholic Fatty Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
