Tuesday Poster Session
Category: Liver
P3811 - Racial Differences in Primary Sclerosing Cholangitis Risk Factors and Outcomes: A Nationwide Study Leveraging a New ICD-10 Code
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Melinda Wang, MD, MHS
University of California San Francisco
San Francisco, CA
Presenting Author(s)
Award: Presidential Poster Award
Melinda Wang, MD, MHS1, Alyssa Harris, MPH2, Sharad Wadhwani, MD, MPH1, Jennifer C.. Lai, MD, MBA1, Jessica B.. Rubin, MD, MPH3
1University of California San Francisco, San Francisco, CA; 2Vizient, Inc., Chicago, IL; 3University of California San Francisco and San Francisco VA Medical Center, San Francisco, CA
Introduction: The natural history, management, and outcomes of primary sclerosing cholangitis (PSC) have traditionally been studied predominantly in White males, as this is the most common affected demographic. Larger retrospective studies of PSC patients, among more diverse populations, have previously been limited by lack of a PSC-specific diagnosis code. We aimed to leverage a new PSC ICD-10 code to characterize racial differences in nationwide contemporary cohort of patients with PSC.
Methods: We used deidentified clinical and administrative data from the Vizient® Clinical Data Base ( >1000 US hospital academic, affiliated, and community hospitals) to identify adult patients with ≥2 inpatient or outpatient encounters with a PSC-specific ICD-10 code (K83.01) or 1 PSC code (10/1/18-1/1/22) and ≥1 cholangitis code (10/1/15-10/1/18). We compared demographic and clinical characteristics between patients who self-identified as Black versus White race using Chi-squared and Wilcoxon rank sum analysis. Multivariable regression was used to associate race with clinical and healthcare utilization outcomes.
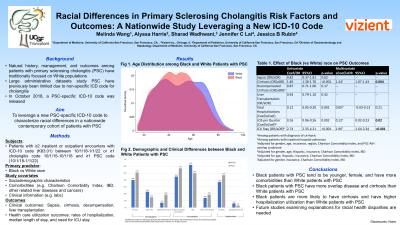
Results: We identified 9,428 patients with PSC: 79% White, 13% Black, 2% Asian, and 6% Other. Compared with White PSC patients, Black PSC patients were more likely to be female, younger, and have a higher Charlson Comorbidity Index (p< 0.001) (
Figure
). Black patients were less likely to have concurrent inflammatory bowel disease (IBD) compared to White patients, but more likely to have overlap syndromes with primary biliary cirrhosis or autoimmune hepatitis (p< 0.001). On multivariable logistic regression, Black race was significantly associated with more hospitalizations (aCoef 0.26, 95%CI 0.11-0.41), longer hospital length of stay (aIRR 1.15, 95%CI 1.06-1.25) and similar rates of transplantation (aOR 0.90, 95%CI 0.75-1.08, p=0.25), even after adjustment for other demographics and disease severity.
Discussion: Black patients with PSC were younger, more likely to be female, and had more comorbidities. Despite adjustment for comorbidities, they had more hospitalizations and longer length of stay when hospitalized. These findings suggest that additional research on optimal diagnosis and management of PSC in Black populations specifically is necessary to reduce healthcare disparities in this disease.

Disclosures:
Melinda Wang, MD, MHS1, Alyssa Harris, MPH2, Sharad Wadhwani, MD, MPH1, Jennifer C.. Lai, MD, MBA1, Jessica B.. Rubin, MD, MPH3. P3811 - Racial Differences in Primary Sclerosing Cholangitis Risk Factors and Outcomes: A Nationwide Study Leveraging a New ICD-10 Code, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Melinda Wang, MD, MHS1, Alyssa Harris, MPH2, Sharad Wadhwani, MD, MPH1, Jennifer C.. Lai, MD, MBA1, Jessica B.. Rubin, MD, MPH3
1University of California San Francisco, San Francisco, CA; 2Vizient, Inc., Chicago, IL; 3University of California San Francisco and San Francisco VA Medical Center, San Francisco, CA
Introduction: The natural history, management, and outcomes of primary sclerosing cholangitis (PSC) have traditionally been studied predominantly in White males, as this is the most common affected demographic. Larger retrospective studies of PSC patients, among more diverse populations, have previously been limited by lack of a PSC-specific diagnosis code. We aimed to leverage a new PSC ICD-10 code to characterize racial differences in nationwide contemporary cohort of patients with PSC.
Methods: We used deidentified clinical and administrative data from the Vizient® Clinical Data Base ( >1000 US hospital academic, affiliated, and community hospitals) to identify adult patients with ≥2 inpatient or outpatient encounters with a PSC-specific ICD-10 code (K83.01) or 1 PSC code (10/1/18-1/1/22) and ≥1 cholangitis code (10/1/15-10/1/18). We compared demographic and clinical characteristics between patients who self-identified as Black versus White race using Chi-squared and Wilcoxon rank sum analysis. Multivariable regression was used to associate race with clinical and healthcare utilization outcomes.
Results: We identified 9,428 patients with PSC: 79% White, 13% Black, 2% Asian, and 6% Other. Compared with White PSC patients, Black PSC patients were more likely to be female, younger, and have a higher Charlson Comorbidity Index (p< 0.001) (
Figure
). Black patients were less likely to have concurrent inflammatory bowel disease (IBD) compared to White patients, but more likely to have overlap syndromes with primary biliary cirrhosis or autoimmune hepatitis (p< 0.001). On multivariable logistic regression, Black race was significantly associated with more hospitalizations (aCoef 0.26, 95%CI 0.11-0.41), longer hospital length of stay (aIRR 1.15, 95%CI 1.06-1.25) and similar rates of transplantation (aOR 0.90, 95%CI 0.75-1.08, p=0.25), even after adjustment for other demographics and disease severity.
Discussion: Black patients with PSC were younger, more likely to be female, and had more comorbidities. Despite adjustment for comorbidities, they had more hospitalizations and longer length of stay when hospitalized. These findings suggest that additional research on optimal diagnosis and management of PSC in Black populations specifically is necessary to reduce healthcare disparities in this disease.

Figure: Figure. Demographic and Clinical Differences between Black and White patients with PSC
Disclosures:
Melinda Wang indicated no relevant financial relationships.
Alyssa Harris indicated no relevant financial relationships.
Sharad Wadhwani indicated no relevant financial relationships.
Jennifer Lai: Flagship Pioneering – Grant/Research Support. Genfit – Consultant. Novo Nordisk – Advisory Committee/Board Member. Pliant – Grant/Research Support.
Jessica Rubin indicated no relevant financial relationships.
Melinda Wang, MD, MHS1, Alyssa Harris, MPH2, Sharad Wadhwani, MD, MPH1, Jennifer C.. Lai, MD, MBA1, Jessica B.. Rubin, MD, MPH3. P3811 - Racial Differences in Primary Sclerosing Cholangitis Risk Factors and Outcomes: A Nationwide Study Leveraging a New ICD-10 Code, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

