Tuesday Poster Session
Category: Liver
P3813 - Predictors of Renal Replacement Therapy Requirement in Cirrhotic Patients Presenting with Acute Renal Failure
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mohammed Hasan, DO
Staten Island University Hospital Northwell Health
Staten Island, NY
Presenting Author(s)
Mohammed Hasan, DO1, Jeffrey Loeffler, MD1, Faris Qaqish, MD2, Ahmad Abou Yassine, MD2, Liliane Deeb, MD2
1Staten Island University Hospital Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Staten Island, NY
Introduction: Renal failure is a well-known and often times, a severe complication in patients with liver cirrhosis. Various renal physiologic changes occur indirectly due to the hyperdynamic circulatory state of cirrhosis, making acute kidney injury (AKI) a common and often deadly problem for patients with decompensated cirrhosis. Patients who require renal replacement therapy (RRT) experience the highest rates of morbidity. There is scarcity of data examining the specific characteristics resulting in RRT requirement in cirrhotic patients presenting with AKI. Our study aimed to explore those particular factors.
Methods: A total of 516 cirrhotic patients presenting with AKI between January 2019 and December 2020 were retrospectively sampled from Northwell Health database. Patients were divided into two groups based on the requirement of RRT during hospital stay (+RRT vs -RRT groups). Data collection of patient demographics, medical history, vital signs, laboratory data, and hospital outcomes were collected and manually identified. Bivariate analysis was used to identify variables associated with patients that required RRT during hospital admission.
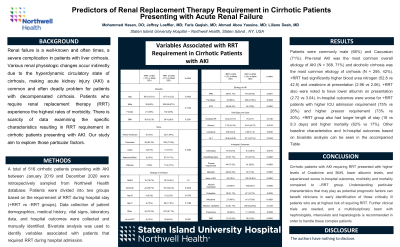
Results: Patients were commonly male (66%) and Caucasian (71%). Pre-renal AKI was the most common overall etiology of AKI (N = 368, 71%) and alcoholic cirrhosis was the most common etiology of cirrhosis (N = 295, 42%). +RRT had significantly higher blood urea nitrogen (52.8 vs 42.5) and creatinine at presentation (2.96 vs 2.06). +RRT also were noted to have lower albumin on presentation (2.72 vs 3.04). In-hospital outcomes were worse for +RRT patients with higher ICU admission requirement (75% vs 26%) and higher pressor requirement (73% vs 20%). +RRT group also had longer length of stay (16 vs 9.3 days) and higher mortality (62% vs 17%). Other baseline characteristics and In-hospital outcomes based on bivariate analysis can be seen in Table 1.
Discussion: Cirrhotic patients with AKI requiring RRT presented with higher levels of Creatinine and BUN, lower albumin levels, and experienced worse in-hospital outcomes, morbidity and mortality compared to –RRT group. Understanding particular characteristics that may play as potential prognostic factors can benefit clinicians in early identification of those critically ill patients who are at highest risk of requiring RRT. Further clinical trials are needed, and a multidisciplinary team with nephrologists, intensivists and hepatologists is recommended in order to handle these complex patients.
Disclosures:
Mohammed Hasan, DO1, Jeffrey Loeffler, MD1, Faris Qaqish, MD2, Ahmad Abou Yassine, MD2, Liliane Deeb, MD2. P3813 - Predictors of Renal Replacement Therapy Requirement in Cirrhotic Patients Presenting with Acute Renal Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Staten Island University Hospital Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Staten Island, NY
Introduction: Renal failure is a well-known and often times, a severe complication in patients with liver cirrhosis. Various renal physiologic changes occur indirectly due to the hyperdynamic circulatory state of cirrhosis, making acute kidney injury (AKI) a common and often deadly problem for patients with decompensated cirrhosis. Patients who require renal replacement therapy (RRT) experience the highest rates of morbidity. There is scarcity of data examining the specific characteristics resulting in RRT requirement in cirrhotic patients presenting with AKI. Our study aimed to explore those particular factors.
Methods: A total of 516 cirrhotic patients presenting with AKI between January 2019 and December 2020 were retrospectively sampled from Northwell Health database. Patients were divided into two groups based on the requirement of RRT during hospital stay (+RRT vs -RRT groups). Data collection of patient demographics, medical history, vital signs, laboratory data, and hospital outcomes were collected and manually identified. Bivariate analysis was used to identify variables associated with patients that required RRT during hospital admission.
Results: Patients were commonly male (66%) and Caucasian (71%). Pre-renal AKI was the most common overall etiology of AKI (N = 368, 71%) and alcoholic cirrhosis was the most common etiology of cirrhosis (N = 295, 42%). +RRT had significantly higher blood urea nitrogen (52.8 vs 42.5) and creatinine at presentation (2.96 vs 2.06). +RRT also were noted to have lower albumin on presentation (2.72 vs 3.04). In-hospital outcomes were worse for +RRT patients with higher ICU admission requirement (75% vs 26%) and higher pressor requirement (73% vs 20%). +RRT group also had longer length of stay (16 vs 9.3 days) and higher mortality (62% vs 17%). Other baseline characteristics and In-hospital outcomes based on bivariate analysis can be seen in Table 1.
Discussion: Cirrhotic patients with AKI requiring RRT presented with higher levels of Creatinine and BUN, lower albumin levels, and experienced worse in-hospital outcomes, morbidity and mortality compared to –RRT group. Understanding particular characteristics that may play as potential prognostic factors can benefit clinicians in early identification of those critically ill patients who are at highest risk of requiring RRT. Further clinical trials are needed, and a multidisciplinary team with nephrologists, intensivists and hepatologists is recommended in order to handle these complex patients.
Disclosures:
Mohammed Hasan indicated no relevant financial relationships.
Jeffrey Loeffler indicated no relevant financial relationships.
Faris Qaqish indicated no relevant financial relationships.
Ahmad Abou Yassine indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Mohammed Hasan, DO1, Jeffrey Loeffler, MD1, Faris Qaqish, MD2, Ahmad Abou Yassine, MD2, Liliane Deeb, MD2. P3813 - Predictors of Renal Replacement Therapy Requirement in Cirrhotic Patients Presenting with Acute Renal Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
