Tuesday Poster Session
Category: Interventional Endoscopy
P3734 - Pancreaticopleural Fistula: A Rare Complication of Pancreatitis Successfully Treated with Endotherapy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ibrar Atiq, MD
United Health Services Hospital
Johnson City, NY
Presenting Author(s)
Ibrar Atiq, MD1, Ali Khan, MD2, Fahad Malik, MD3, Ali Marhaba, MD1, Amanke Oranu, MD1
1United Health Services Hospital, Johnson City, NY; 2United Health Services Hospitals, Binghamton, NY; 3United Health Services, Binghamton, NY
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of acute or chronic pancreatitis and an unusual cause of pleuropulmonary disease with an incidence of 0.4%. In patients with chronic pancreatitis and recurrent pleural effusion, the possibility of a PFF should always be considered.
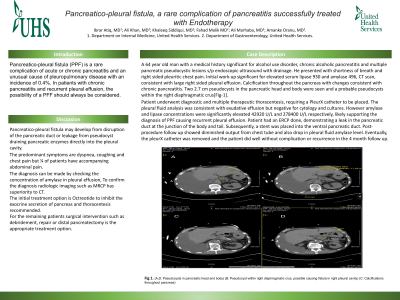
Case Description/Methods: A 64 year old man with a medical history significant for alcohol use disorder, chronic alcoholic pancreatitis and multiple pancreatic pseudocystic lesions s/p endoscopic ultrasound with drainage. He presented with shortness of breath and right sided pleuritic chest pain. Initial work-up significant for elevated serum lipase 930 and amylase 496, CT scan, consistent with large right sided pleural effusion. Calcification throughout the pancreas with changes consistent with chronic pancreatitis. Two 2.7 cm pseudocysts in the pancreatic head and body were seen and a probable pseudocysts within the right diaphragmatic crus[Fig-1].
Patient underwent diagnostic and multiple therapeutic thoracentesis, requiring a PleurX catheter to be placed. The pleural fluid analysis was consistent with exudative effusion but negative for cytology and cultures. However amylase and lipase concentrations were significantly elevated 42920 U/L and 278400 U/L respectively, likely supporting the diagnosis of PPF causing recurrent pleural effusion. Patient had an ERCP done, demonstrating a leak in the pancreatic duct at the junction of the body and tail. Subsequently, a stent was placed into the ventral pancreatic duct. Post-procedure follow up showed diminished output from chest tube and also drop in pleural fluid amylase level. Eventually, the pleurX catheter was removed and the patient did well without complication or recurrence in the 4 month follow up.
Discussion: Pancreaticopleural fistula may develop from disruption of the pancreatic duct or leakage from pseudocyst draining pancreatic enzymes directly into the pleural cavity.
The predominant symptoms are dyspnea, coughing and chest pain but ¼ of patients have accompanying abdominal pain.
The diagnosis can be made by checking the concentration of amylase in pleural effusion, To confirm the diagnosis radiologic imaging such as MRCP has superiority to CT.
The initial treatment option is Octreotide to inhibit the exocrine secretion of pancreas and thoracentesis recommended.
For the remaining patients surgical intervention such as debridement, repair or distal pancreatectomy is the appropriate treatment option.

Disclosures:
Ibrar Atiq, MD1, Ali Khan, MD2, Fahad Malik, MD3, Ali Marhaba, MD1, Amanke Oranu, MD1. P3734 - Pancreaticopleural Fistula: A Rare Complication of Pancreatitis Successfully Treated with Endotherapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1United Health Services Hospital, Johnson City, NY; 2United Health Services Hospitals, Binghamton, NY; 3United Health Services, Binghamton, NY
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of acute or chronic pancreatitis and an unusual cause of pleuropulmonary disease with an incidence of 0.4%. In patients with chronic pancreatitis and recurrent pleural effusion, the possibility of a PFF should always be considered.
Case Description/Methods: A 64 year old man with a medical history significant for alcohol use disorder, chronic alcoholic pancreatitis and multiple pancreatic pseudocystic lesions s/p endoscopic ultrasound with drainage. He presented with shortness of breath and right sided pleuritic chest pain. Initial work-up significant for elevated serum lipase 930 and amylase 496, CT scan, consistent with large right sided pleural effusion. Calcification throughout the pancreas with changes consistent with chronic pancreatitis. Two 2.7 cm pseudocysts in the pancreatic head and body were seen and a probable pseudocysts within the right diaphragmatic crus[Fig-1].
Patient underwent diagnostic and multiple therapeutic thoracentesis, requiring a PleurX catheter to be placed. The pleural fluid analysis was consistent with exudative effusion but negative for cytology and cultures. However amylase and lipase concentrations were significantly elevated 42920 U/L and 278400 U/L respectively, likely supporting the diagnosis of PPF causing recurrent pleural effusion. Patient had an ERCP done, demonstrating a leak in the pancreatic duct at the junction of the body and tail. Subsequently, a stent was placed into the ventral pancreatic duct. Post-procedure follow up showed diminished output from chest tube and also drop in pleural fluid amylase level. Eventually, the pleurX catheter was removed and the patient did well without complication or recurrence in the 4 month follow up.
Discussion: Pancreaticopleural fistula may develop from disruption of the pancreatic duct or leakage from pseudocyst draining pancreatic enzymes directly into the pleural cavity.
The predominant symptoms are dyspnea, coughing and chest pain but ¼ of patients have accompanying abdominal pain.
The diagnosis can be made by checking the concentration of amylase in pleural effusion, To confirm the diagnosis radiologic imaging such as MRCP has superiority to CT.
The initial treatment option is Octreotide to inhibit the exocrine secretion of pancreas and thoracentesis recommended.
For the remaining patients surgical intervention such as debridement, repair or distal pancreatectomy is the appropriate treatment option.

Figure: (A,D: Pseudocysts in pancreatic head and body) (B: Pseudocyst within right diaphragmatic crus, possible causing fistula in right pleural cavity) (C: Calcifications throughout pancreas)
Disclosures:
Ibrar Atiq indicated no relevant financial relationships.
Ali Khan indicated no relevant financial relationships.
Fahad Malik indicated no relevant financial relationships.
Ali Marhaba indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Ibrar Atiq, MD1, Ali Khan, MD2, Fahad Malik, MD3, Ali Marhaba, MD1, Amanke Oranu, MD1. P3734 - Pancreaticopleural Fistula: A Rare Complication of Pancreatitis Successfully Treated with Endotherapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
