Tuesday Poster Session
Category: Interventional Endoscopy
P3746 - Transcolonic Drainage of Walled-Off Pancreatic Necrosis: A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MK
Muhammad Zarrar Khan, MD
Henry Ford Medical Center
Detroit, MI
Presenting Author(s)
Award: Presidential Poster Award
Muhammad Zarrar Khan, MD1, Mark Obri, MD2, Ammad Chaudhary, MD2, Mazen Elatrache, MD2, Sumit Singla, MD2, Andrew Watson, MD2, Tobias Zuchelli, MD2
1Henry Ford Medical Center, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Walled-off pancreatic necrosis (WOPN) is a chronic and rare complication of necrotizing pancreatitis. Collections that require drainage, endoscopic necrosectomy has emerged as the standard of treatment. Frequently, drainage is achieved via a trans-gastric or a trans-duodenal approach. Here, we present a case of complicated pericolonic WOPN managed with a lumen-apposing metal stent. (LAMS)
Case Description/Methods: A 48-year-old male, with a history of hyperlipidemia, presented to an outside hospital with abdominal pain and vomiting for one week. He denied smoking and active drinking. Presenting hemodynamics were stable. Labs revealed elevated lipase >1200 U/L. Computed Tomography (CT) scan of the abdomen revealed acute pancreatitis without fluid collections. His course was complicated by multiorgan failure; which prompted transfer to our center for escalation of care.
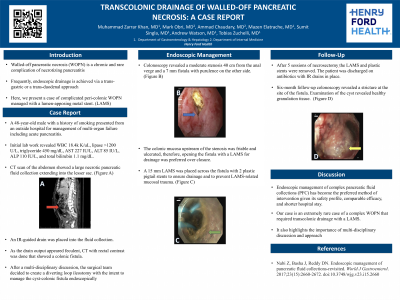
He continued to deteriorate, and a repeat CT 3 weeks later showed a large WOPN. (1A) He underwent IR-guided drain placement into the fluid collection. As the drain output appeared feculent, CT with rectal contrast was performed and demonstrated a colonic fistula. After a multi-disciplinary discussion, the surgical team created a diverting loop ileostomy with the intent to manage the cyst-colonic fistula endoscopically. Colonoscopy revealed a moderate stenosis 40 cm from the anal verge and a 7 mm fistula with purulence on the other side. (1B) Mucosa upstream of the stenosis was friable and ulcerated, and opening the fistula with a LAMS for drainage was preferred over closure. A 15 mm LAMS was placed across the fistula with 2 plastic pigtail stents to ensure drainage and prevent LAMS-related mucosal trauma. (1C) After 5 sessions of necrosectomy the LAMS and plastic stents were removed. The patient was discharged on antibiotics with IR drains in place. A 6-month follow-up revealed a collapse of the cyst (1D), stricture at the site of the fistula with healthy granulation tissue at the cyst.
Discussion: This case emphasizes the importance of multi-disciplinary discussions and utilizing all tools in our endoscopic toolkit to ensure the appropriate resolution of complex pancreatic fluid collections (PFC). Endoscopic management, particularly through EUS guided transgastric or transduodenal drainage and necrosectomy, has become the preferred method of intervention for PFCs. However, in cases such as this one, where a colonic fistula is present, successful trans-colonic drainage using a LAMS can be a valuable tool in managing the condition.

Disclosures:
Muhammad Zarrar Khan, MD1, Mark Obri, MD2, Ammad Chaudhary, MD2, Mazen Elatrache, MD2, Sumit Singla, MD2, Andrew Watson, MD2, Tobias Zuchelli, MD2. P3746 - Transcolonic Drainage of Walled-Off Pancreatic Necrosis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Muhammad Zarrar Khan, MD1, Mark Obri, MD2, Ammad Chaudhary, MD2, Mazen Elatrache, MD2, Sumit Singla, MD2, Andrew Watson, MD2, Tobias Zuchelli, MD2
1Henry Ford Medical Center, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Walled-off pancreatic necrosis (WOPN) is a chronic and rare complication of necrotizing pancreatitis. Collections that require drainage, endoscopic necrosectomy has emerged as the standard of treatment. Frequently, drainage is achieved via a trans-gastric or a trans-duodenal approach. Here, we present a case of complicated pericolonic WOPN managed with a lumen-apposing metal stent. (LAMS)
Case Description/Methods: A 48-year-old male, with a history of hyperlipidemia, presented to an outside hospital with abdominal pain and vomiting for one week. He denied smoking and active drinking. Presenting hemodynamics were stable. Labs revealed elevated lipase >1200 U/L. Computed Tomography (CT) scan of the abdomen revealed acute pancreatitis without fluid collections. His course was complicated by multiorgan failure; which prompted transfer to our center for escalation of care.
He continued to deteriorate, and a repeat CT 3 weeks later showed a large WOPN. (1A) He underwent IR-guided drain placement into the fluid collection. As the drain output appeared feculent, CT with rectal contrast was performed and demonstrated a colonic fistula. After a multi-disciplinary discussion, the surgical team created a diverting loop ileostomy with the intent to manage the cyst-colonic fistula endoscopically. Colonoscopy revealed a moderate stenosis 40 cm from the anal verge and a 7 mm fistula with purulence on the other side. (1B) Mucosa upstream of the stenosis was friable and ulcerated, and opening the fistula with a LAMS for drainage was preferred over closure. A 15 mm LAMS was placed across the fistula with 2 plastic pigtail stents to ensure drainage and prevent LAMS-related mucosal trauma. (1C) After 5 sessions of necrosectomy the LAMS and plastic stents were removed. The patient was discharged on antibiotics with IR drains in place. A 6-month follow-up revealed a collapse of the cyst (1D), stricture at the site of the fistula with healthy granulation tissue at the cyst.
Discussion: This case emphasizes the importance of multi-disciplinary discussions and utilizing all tools in our endoscopic toolkit to ensure the appropriate resolution of complex pancreatic fluid collections (PFC). Endoscopic management, particularly through EUS guided transgastric or transduodenal drainage and necrosectomy, has become the preferred method of intervention for PFCs. However, in cases such as this one, where a colonic fistula is present, successful trans-colonic drainage using a LAMS can be a valuable tool in managing the condition.

Figure: A (red arrow): A large necrotic WOPN extending into the lesser sac
B (blue arrow): A 7 mm cysto-colic fistula with purulent material
C (green arrow): LAMS with pigtail stents
D (yellow arrow): Cyst with healthy granulation tissue
B (blue arrow): A 7 mm cysto-colic fistula with purulent material
C (green arrow): LAMS with pigtail stents
D (yellow arrow): Cyst with healthy granulation tissue
Disclosures:
Muhammad Zarrar Khan indicated no relevant financial relationships.
Mark Obri indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Sumit Singla: Boston Scientific – Consultant.
Andrew Watson indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Muhammad Zarrar Khan, MD1, Mark Obri, MD2, Ammad Chaudhary, MD2, Mazen Elatrache, MD2, Sumit Singla, MD2, Andrew Watson, MD2, Tobias Zuchelli, MD2. P3746 - Transcolonic Drainage of Walled-Off Pancreatic Necrosis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

